A Guide to HIV and Drug Rehabilitation
In this guide:
- What is HIV?
- How is HIV spread?
- Who is most likely to contract HIV?
- How does drug use affect the symptoms and the outcome of HIV infection?
- How can someone reduce the risk of spreading the infection?
- Why is attending drug rehab crucial for people with HIV?
- How common is it for people in rehab to also have an HIV infection?
- Does having HIV disqualify a person from attending rehab?
- Are people with HIV separated from those who are uninfected in a rehab center?
- Is rehab different for people with HIV versus those without HIV?
- What special treatment do people with HIV get in rehab?
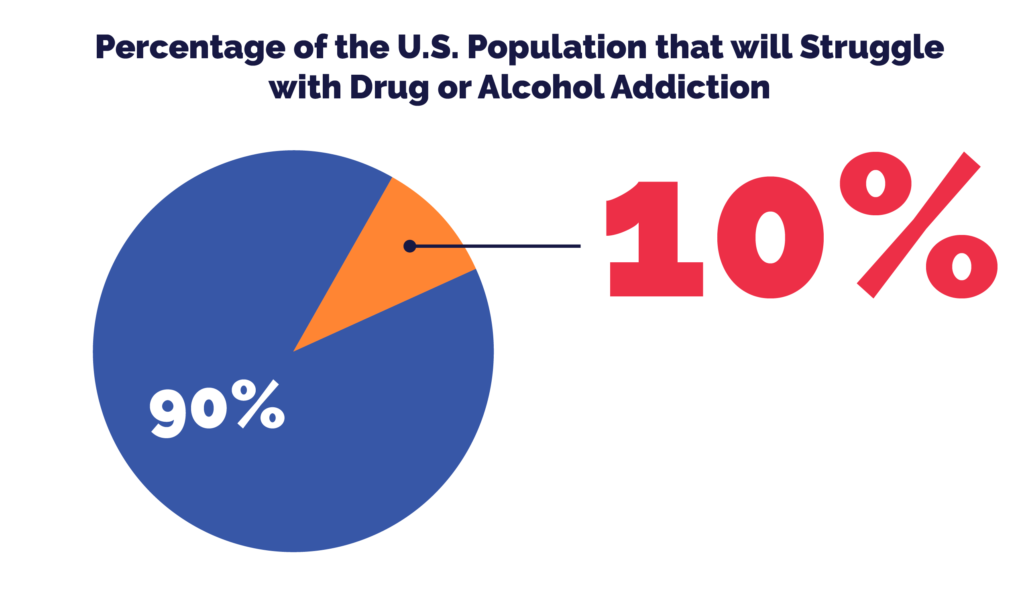
10% of the U.S. population will struggle with drug or alcohol addiction at some point during their lives. Drug abusers, however, have a heightened risk of contracting STIs and other infections as a result of drug abuse. Those who engage in drug use and other high-risk, addictive behaviors are at an increased risk of becoming infected with HIV or hepatitis. These blood-borne illnesses are incredibly severe, painful, and life-threatening. The following guide will explain how drug addiction increases HIV rates, and how a rehabilitation center can help someone with HIV obtain adequate treatment for substance abuse disorder.
What is HIV?
HIV stands for human immunodeficiency virus. The disease infects the body’s immune cells or T-cells. These cells are vital for fighting off infections from bacteria and viruses. HIV destroys the T-cells and lowers the amount of these disease-fighting cells in the body over a period of time. As a result, a person infected with HIV has an incredibly difficult time fighting off viral and bacterial infections. A mild case of pneumonia for a healthy person can be devastating and deadly for someone who is HIV positive.
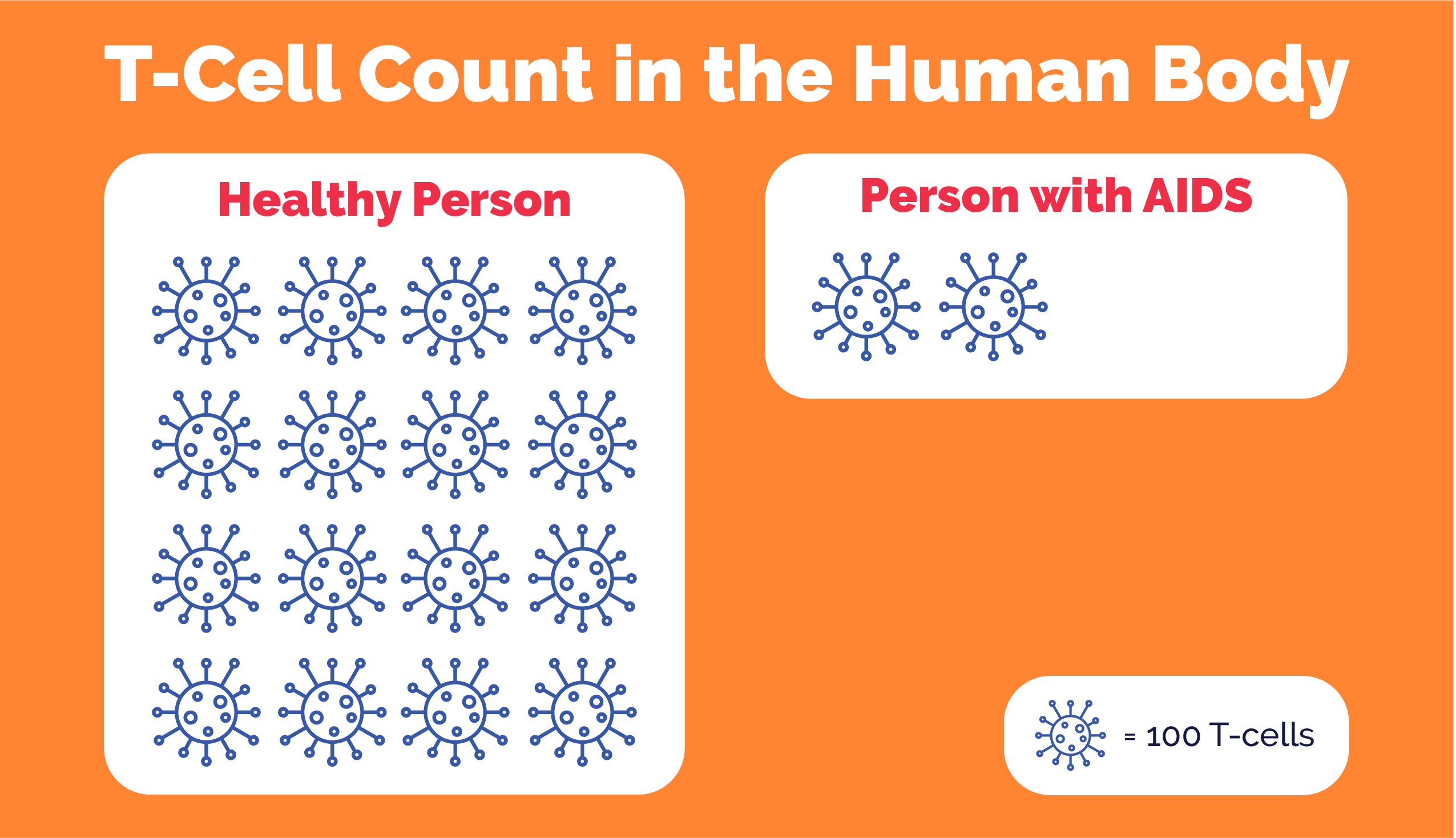
As HIV progresses, it becomes AIDS, or acquired immune deficiency syndrome. An AIDS diagnosis means that the body is unable to fight off any infection or illness. A healthy person has a T-cell count of between 500 and 1600. When someone with HIV has a T-cell count of 200 or less, the disease is in its final stages and is considered AIDS.
Having HIV does not automatically mean that the disease will progress to AIDS, though. With quick intervention and antiretroviral therapy (ART), the disease can be slowed or halted from proceeding all the way to the AIDS stage.
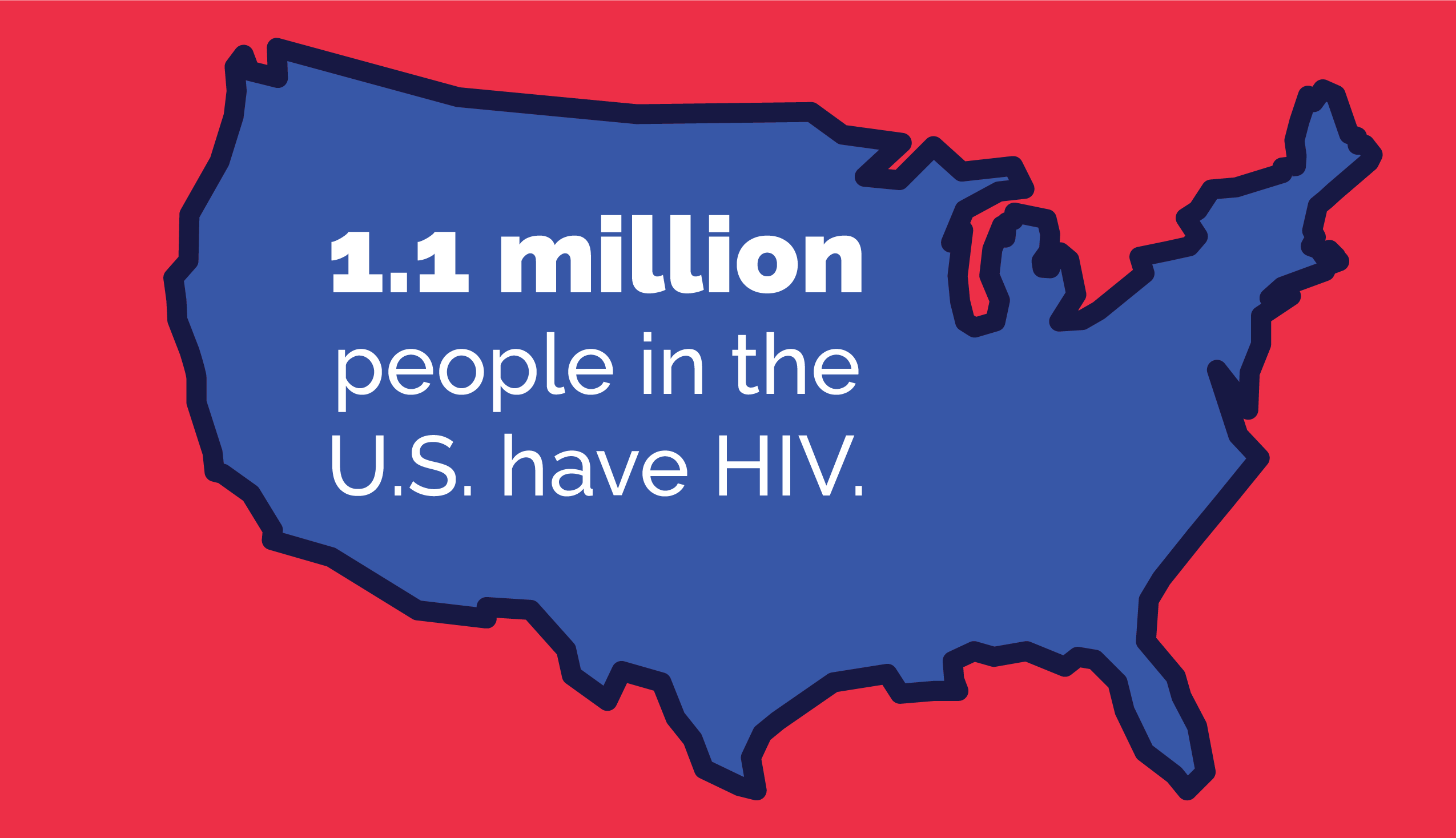
HIV is a viral infection that is spread through either blood or other bodily fluids. 1.1 million people in the U.S. have HIV. The virus is spread in one of two ways:
- When someone injects drugs and shares used needles or other contaminated drug equipment.
- When people engage in unprotected sex with someone who is infected with the virus.
Drug users are at incredibly high risk of contracting HIV. Drug and alcohol use impairs judgment significantly and drug users will often share dirty needles and engage in unprotected sex. Also, women who are infected with HIV can pass the disease on to their baby in utero, and while breastfeeding. In addition, drug use will mask some of the symptoms of HIV. A user may not realize that they are in the early stages of the disease and won’t get initial treatment.
There is no cure for HIV. But early intervention and treatment can slow the progress of the illness and prevent someone from contracting AIDS, the later deadly stage of HIV infection.
Studies from 2005 to 2009 found the following rates of HIV and drug use:
- One in three people with HIV either used drugs or engaged in binge drinking
- 16% of HIV transmission happened because of intravenous drug use
- 84% of HIV transmission occurred because of unprotected sex
- 24% of people with HIV were candidates for drug addiction treatment
Because drug use increases the practice of sharing dirty needles and having unprotected sex, drug addiction treatment and rehab significantly reduce the transmission rates of HIV.
Who is most likely to contract HIV?
HIV and drug use are major public health concerns for the United States and a lack of drug addiction treatment increases the rates of HIV. HIV rates are highest in metropolitan centers. The southeastern part of the U.S. has the highest rates of people living with HIV. But, if population density were accounted for, then the Northeast has the highest rates of people living with the disease.
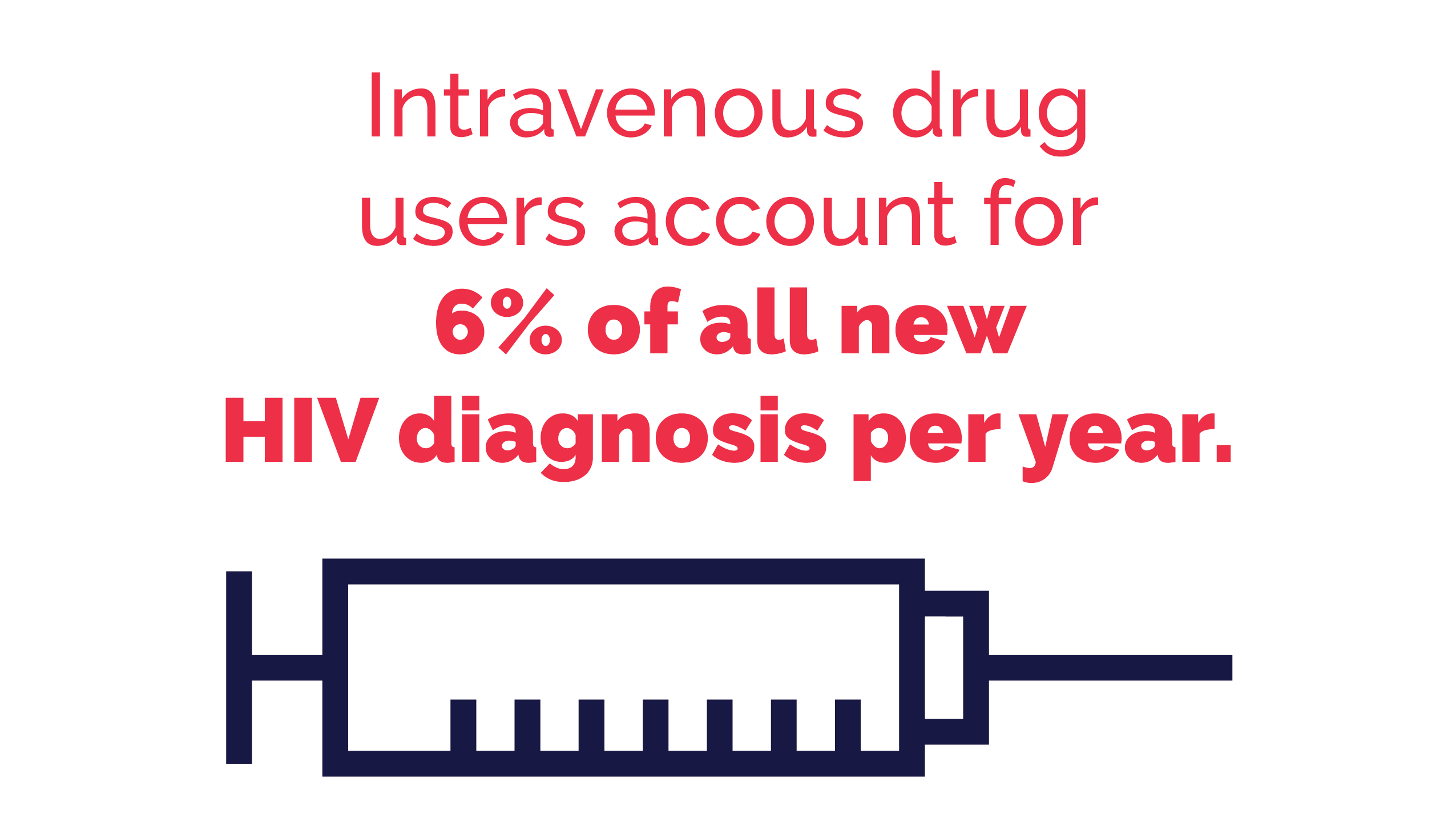
Also, the heroin epidemic in the Northeastern part of the country is contributing to the spread of HIV. Intravenous drug users account for 6% of all new HIV diagnosis per year. Increasing access to drug rehabilitation can significantly reduce the spread of the illness in vulnerable populations.
- One in three people with HIV either used drugs or engaged in binge drinking
- 16% of HIV transmission happened because of intravenous drug use
- 84% of HIV transmission occurred because of unprotected sex
- 24% of people with HIV were candidates for drug addiction treatment
Drug users are at incredibly high risk of contracting HIV. Drug and alcohol use impairs judgment significantly and drug users will often share dirty needles and engage in unprotected sex. Also, women who are infected with HIV can pass the disease on to their baby in utero, and while breastfeeding. In addition, drug use will mask some of the symptoms of HIV. A user may not realize that they are in the early stages of the disease and won’t get initial treatment.
There is no cure for HIV. But early intervention and treatment can slow the progress of the illness and prevent someone from contracting AIDS, the later deadly stage of HIV infection.
Studies from 2005 to 2009 found the following rates of HIV and drug use:
- Black men who engage in male-to-male sexual contact have the highest risk of HIV infection.
- Latina women who engage in heterosexual contact have the lowest rates of HIV infection.
- In 2015, there were an estimated 38,500 new reported cases of HIV infection.
- Annual numbers of diagnosis have been decreasing since 2011.
- One in seven people with HIV do not know they are infected.
- HIV is the ninth leading cause of death for people ages 25 to 44.
- There are 36.7 million people around the world living with HIV.
Prevalence of HIV in California
According to 2018 data, 131,013 Californians are living with HIV. During 2018, 4,712 people in California received an HIV diagnosis. For every 100,000 residents of California, 396 had HIV, compared to 375 per 100,000 people in the United States as a whole.
Of those with HIV in California, 88.2% are men, and 11.8% are women. The rates of HIV among Californians, by race, were as follows:
- Black- 16.6%
- Hispanic/Latino- 38.1%
- White- 37.0%
HIV prevalence, broken down by age, shows the following trends in California:
In 2018, 1,709 Californians died from HIV, with males making up 87.3% of deaths and females accounting for the remaining 12.7%. Of those with HIV living in California, 76% received treatment. Among women, 22.4% who contracted HIV did so through injecting drugs, compared to only 4.6% of men. While men may be more likely to have HIV, women seem to be more at risk of contracting it through drug use.
How does drug use affect the symptoms and the outcome of HIV infection?
Drug use worsens the spread of HIV in several different ways. People struggling with drug addiction may not realize that they are sick. Drug use can mask many of the symptoms of a viral infection such as HIV. Drug use also weakens the body’s immune system, worsening the onset of the disease.
Because users do not know they are sick, continued drug abuse makes it easier for the HIV infection to enter the brain and cause significant nerve cell injury. Nerve cell injury leads to cognitive impairment and other problems with memory and decision making. Also, drug and alcohol abuse damages the liver, making it harder for those with HIV to fight off liver infections and cancers. Infected drug users can also spread the disease to a sexual partner or someone they share needles or other contaminated drug equipment with.
People who engage in high-risk behaviors can do several things to prevent the risk of contracting and spreading HIV.
Post-exposure prophylaxis (PEP) is the practice of taking antiretroviral medicines to prevent infection after being exposed to HIV. PEP is used within the first 72 hours after exposure and should only be used in an emergency.
Pre-exposure prophylaxis or PrEP is when someone who is at risk of contracting HIV takes a daily dose of HIV medications to prevent infection. PrEP is effective at preventing disease in people who abuse drugs.
Because HIV is a disease of urbanization, many cities across the U.S. engage in the practice of harm reduction. Clean needle exchanges, medical services, and safe injection sites are all harm reduction practices to help prevent the spread of HIV in the drug community.
Regular testing for HIV is also an effective way of preventing the spread of the infection in at-risk populations. But, the most significant way to avoid contraction and spreading of the disease is through drug abstinence, drug treatment, and rehabilitation. The link between drug addiction and HIV infection cannot be understated. Treating people for substance abuse is a highly effective way to stop the spread of HIV, and also slow the progression of the disease in someone who is already infected. But not every rehabilitation center is equipped to handle patients with HIV or AIDS infections.
Drug and alcohol abuse will weaken an otherwise healthy person’s immune system. Drug abuse and excessive, chronic drinking can harm different bodily systems and lead to cancers, infections, and other diseases. Also, the life of a drug addict is disorganized and chaotic.
HIV significantly weakens immunity and destroys infection-fighting T-cells in the body. Antiretroviral drugs must be regimented and taken on strict schedules to maximize their effectiveness. Drug rehab is crucial for people with HIV because it will help them to lead a healthier, more organized lifestyle, halting the progression of the disease and prolonging their lives. Getting people with HIV into drug rehab will also stop the spread of infection throughout the drug community.

How common is it for people in rehab to also have an HIV infection?
People in rehab who also have HIV are in the minority. Unfortunately, many drug addicts do not know that they have HIV. Despite harm reduction strategies, it is still difficult for many people, especially those who are infected, to access safe and effective drug rehabilitation. Also, people with HIV or any other special physical health needs require a different approach to treatment.
Does having HIV disqualify a person from attending rehab?
Anyone who is willing to get treatment for their drug addiction can find the resources and the help they need to get clean. People with HIV will not be turned away from a rehabilitation center on the basis of having an infection, that would be considered discrimination, and it is illegal in the U.S.
But, those with HIV require a rehabilitation center that has a high rate of medical professionals on the staff. People in rehab who also have an HIV infection must have access to high-quality medical care to get the infection under control. For people with HIV and AIDs who wish to attend drug rehab, they need to choose a facility with a high rate of nurses and physicians on-site.

Are people with HIV separated from those who are uninfected in a rehab center?
People living with HIV who attend rehab are not separated from the uninfected as a discriminatory act. But, people with HIV may find it beneficial to participate in group therapy sessions and other rehabilitative activities with people who also have HIV. This is a support measure and not an act of separation because of HIV stigma or discrimination.
Is rehab different for people with HIV versus those without HIV?
People without HIV or other disabilities do not need to look for a facility that will meet their medical needs. People who are not disabled have more choices when it comes to picking a qualified rehab center to help them manage their substance abuse disorder.
People with HIV and AIDS who attend rehab need comprehensive, integrated care for managing both the infection and the substance abuse disorder. However, the treatment and management of drug addiction are the same for those with HIV and those without. Medical detox, group and one-on-one therapy, and individualized aftercare plans are effective ways to treat drug addiction in infected and non-infected persons alike.
People with HIV have significant medical needs. Every person who attends rehab and also has HIV is going to be at a different stage in the disease. Chronic, intravenous drug use and polydrug use can also cloud HIV symptoms and hasten the progression of the illness. Those who enter rehab with an HIV infection will require meticulous care to lessen symptoms and prevent the disease from getting worse.
Also, HIV discrimination and the stigma surrounding infection can worsen comorbid mental health conditions and weaken a person’s resolve to stay clean. Many people with HIV will refuse treatment because of the fear of stigma and discrimination. For those who are infected, it’s important to find a rehabilitation center that is familiar with the needs of HIV patients and can cater to those needs effectively.
Discrimination marginalizes people socially, economically, and legally, leading them to engage in risky behaviors like drug addiction or to ignore their health. Drug treatment centers with knowledgeable staff can help people with disabilities overcome these stigmas and get the help they need for drug abuse and comorbid mental health conditions stemming from depression and anxiety related to discrimination.
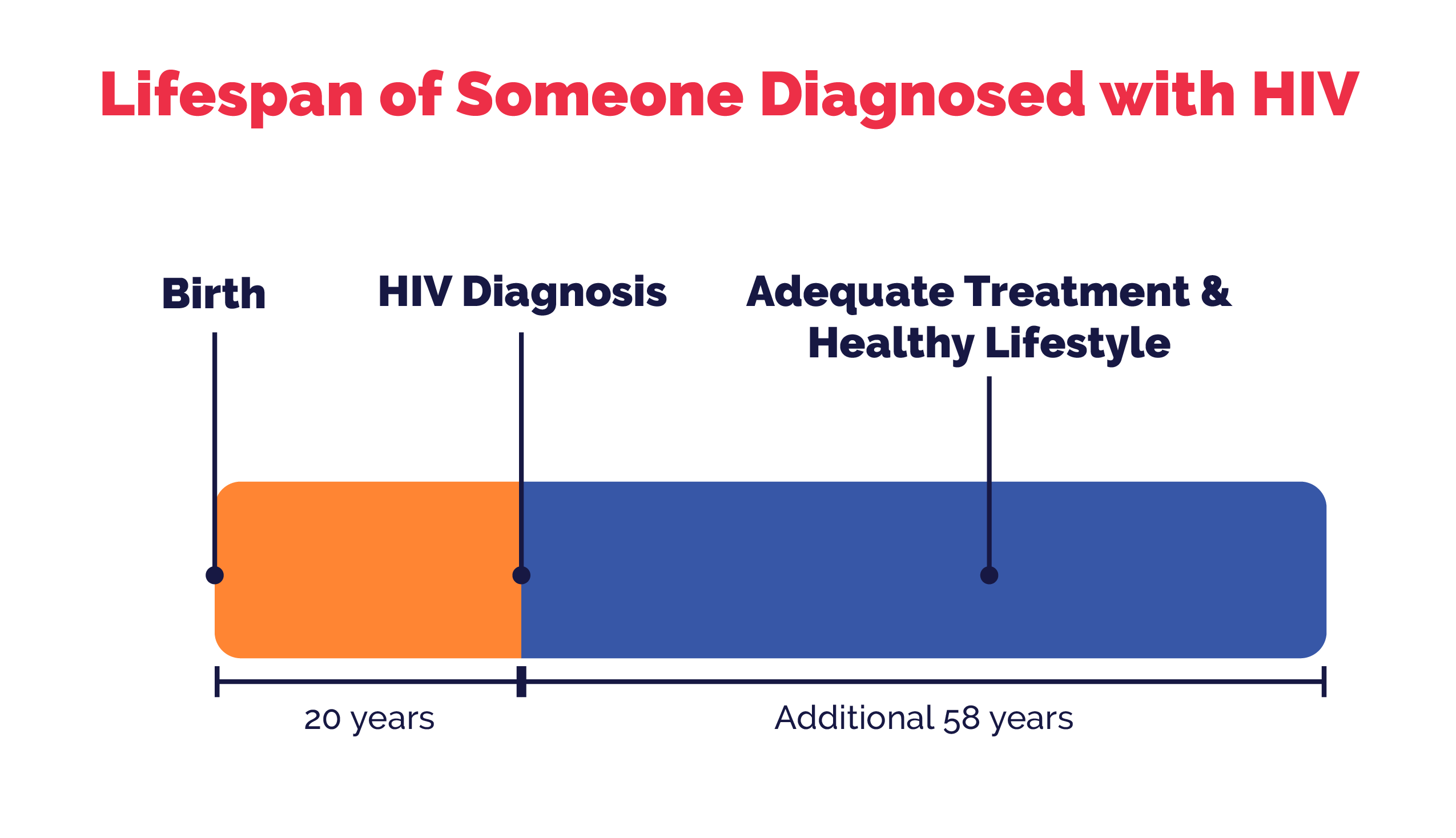
Although there is no cure for HIV, there are effective treatment methods available and the disease does not have to be a life sentence. With adequate treatment, people with HIV can go on to live a full life. Studies show that for someone diagnosed with HIV at 20 years old, they will live an additional 58 years if they receive adequate treatment and commit to living a healthy lifestyle.
To prevent the spread of HIV, it’s crucial that people with drug addiction seek help and attend a licensed rehabilitation center. Staff that is trained to help people with HIV and substance abuse disorder can effectively treat patients and assist them in managing the complex and distressing emotions surrounding a diagnosis like HIV. If you or someone you love is struggling with substance abuse and has an HIV positive diagnosis, it’s never too late to reach out for help.
Treatment Outcomes for Individuals with an Addiction and HIV
Addiction can worsen the health of someone with HIV and make it difficult to live a safe, productive life, but treatment can reduce health risks and improve the quality of life for these patients. Fortunately, researchers have evaluated the effects of treatment for patients with HIV and addiction, and outcomes have been positive.
For example, one study evaluated the effects of an implant of a medication called naltrexone on patients with HIV and opiate addictions. Results showed that having an implant improved the health of those with HIV and reduced the risk of relapse, health problems, and fatal overdoses. Being in treatment for addiction can be life-saving for those with HIV.
Being involved with addiction treatment can also reduce a person’s risk of contracting HIV. Keep in mind that drug use can also lead to risky sexual behaviors, such as sharing needles or having unprotected sex. Entering treatment helps people to change their behaviors, thereby placing themselves at less risk. In fact, a 2018 study in the publication Drug and Alcohol Dependence found that a brief intervention with a therapist, combined with a follow-up intervention three months later, decreased risky sexual behaviors among drug users. This means that treatment not only improves health for those with HIV but may prevent drug users from contracting HIV at all.
Treatment does work, and it can improve health for those living with both HIV and addiction. If you are seeking addiction treatment in the Southern California area, Mission Harbor Behavioral Health offers substance abuse and mental health treatment for both adults and adolescents. We can provide various treatment tracks, and our goal is to design a customized plan that meets each client’s individual needs and addresses all the issues surrounding their addiction. We also offer multiple levels of care, including a partial hospitalization program for those undergoing detox and withdrawal, and intensive outpatient services with flexible scheduling options. We accept most major insurance providers, and we can offer a schedule that meets the needs of working professionals. Contact us today to get started.
Updated content on 4/24/2021
This guide is intended to be informational. If you are considering help for you or your loved one and would like more information, please consult a medical professional or licensed treatment facility.

