A Guide to Recovery and Assistance Options for Mental Health and Addiction
In this guide:
- Detox Facilities
- Individual Psychologists
- Psychiatrist
- Peer Specialists
- Homeless Shelters
- Battered Women Shelters
- Court Ordered Programs
- 12-Step Meetings
- Alcoholics Anonymous or AA
- Narcotics Anonymous, or N.A.
- Gamblers Anonymous or G.A.
- Pain Management Clinics
- Church and Other Religious Institutions
- Licensed Marriage and Family Therapists, and Marriage and Family Therapists (MFT)
- Clinical Social Workers (CSW)
- Outpatient Treatment
- Inpatient Treatment Programs
- Residential Treatment Programs
- Sober Living
- Department of Veterans Affairs (VA)
- Nursing Homes for the Elderly
- Partial Hospitalization (PHP)
- Community Mental Health Centers
- Acute Residential Treatment
- Intensive Outpatient Programs (IOP)
- Drug Replacement Centers

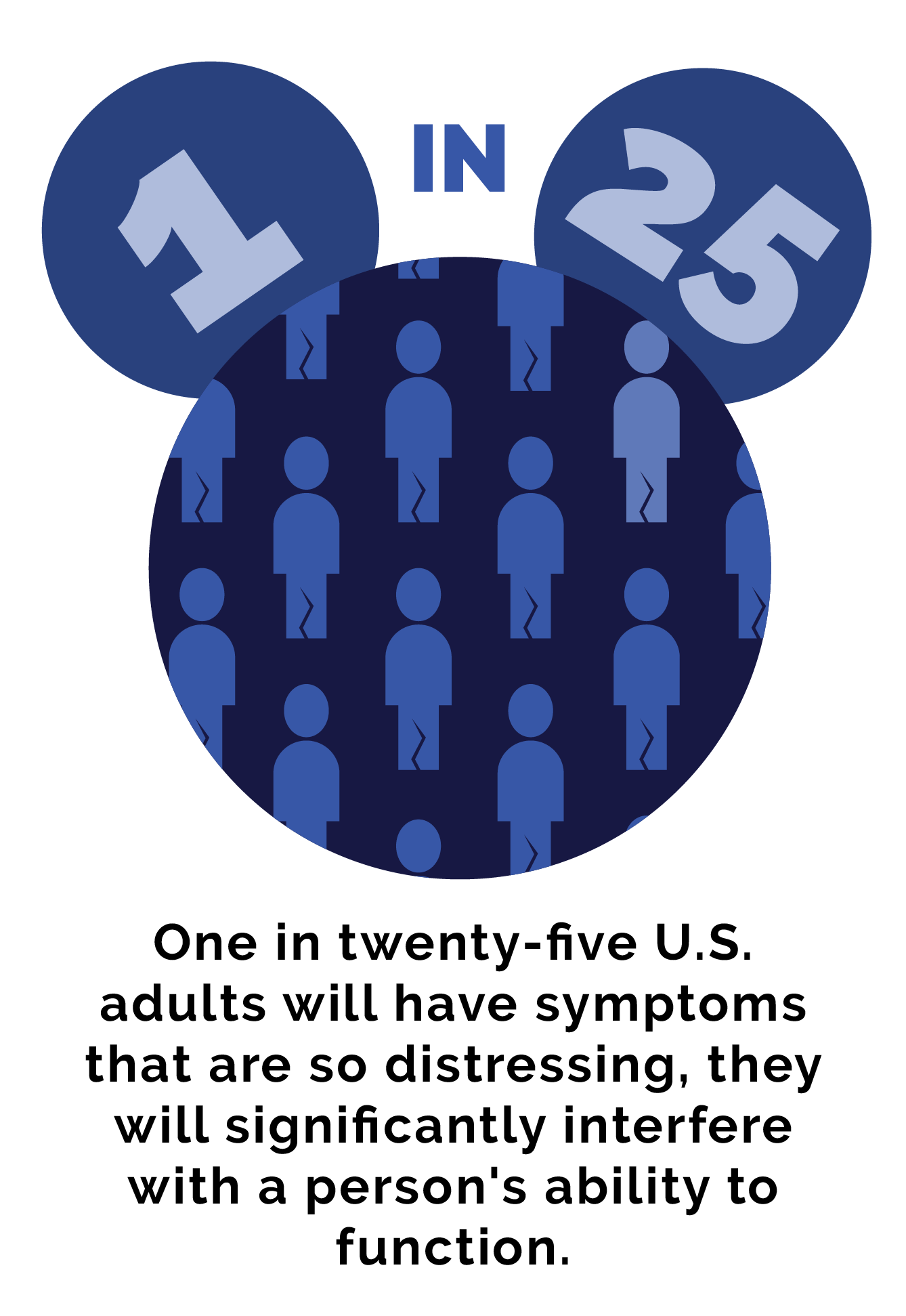
In a given year, one in five U.S. adults will experience the symptoms of a diagnosable mental health condition.
One in twenty-five U.S. adults will have symptoms that are so distressing, they will significantly interfere with a person’s ability to function.
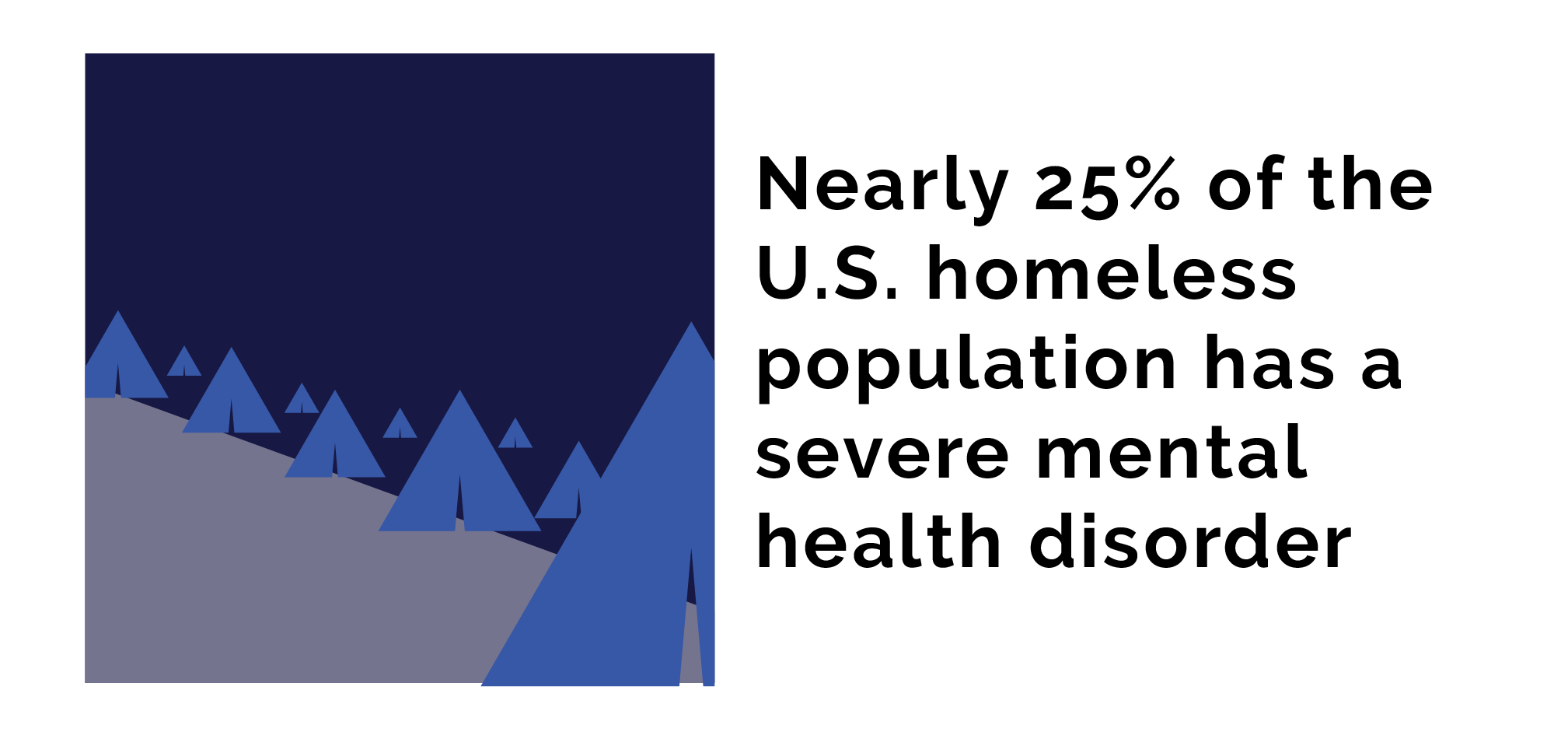
Untreated mental health disorders are a massive contributor to the nation’s homeless population, with estimates stating that nearly 25% of the U.S. homeless population has a severe mental health disorder.
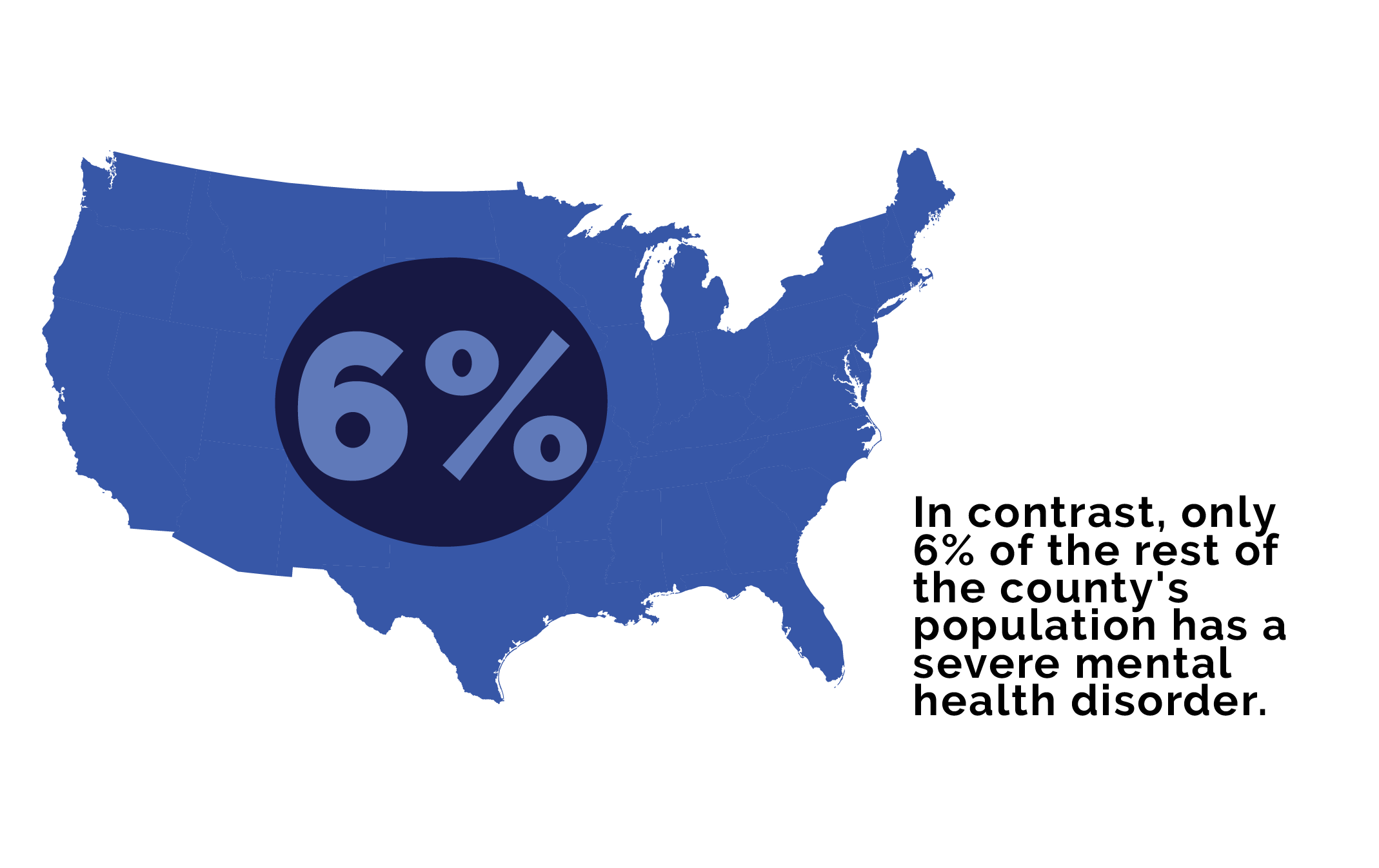 In contrast, only 6% of the rest of the county’s population has a severe mental health disorder.
In contrast, only 6% of the rest of the county’s population has a severe mental health disorder.
Mental health disorders are also a major contributor to drug and alcohol abuse rates. Unfortunately, barriers to treatment access for mental health conditions and societal stigma make it difficult for patients to obtain adequate care and find relief from distressing and painful symptoms. For many, drugs and alcohol are far more accessible than comprehensive, safe, and appropriate medical care for mental health. Stimulants can quickly alleviate the fatigue and brain fog of depression, while alcohol can calm panic attacks and anxiety. People who struggle with mood and anxiety disorders are twice as likely as the general population to develop drug or alcohol use disorders.
Treating addiction and treating mental health disorders simultaneously with integrated treatment models is critical for helping patients achieve sobriety and find relief from distressing symptoms. The following guide will address the various counseling, therapeutic, and medical treatment methods that can be used to treat mental health and substance use disorders, or dual diagnosis.
Detox facilities are for people who are addicted to drugs or alcohol and are trying to quit.
A patient’s stay in a detox facility can vary significantly depending on the type of substances they are addicted to, and how long they’ve been addicted. Some drugs can take several days, to weeks to clear out from the body, and a person’s physical health, gender, weight, and metabolism can all influence the detox timeline.
A detox facility is typically staffed with a range of doctors and clinicians. Patients will have access to psychologists, psychiatrists, doctors, nurses, therapists, counselors, and social workers who specialize in treating drug addiction. These facilities must comply with state regulations.
Usually, a detox facility is located in a hospital or clinical setting. Patients may stay on-site during the detox process, or attend detox at scheduled times during the withdrawal timeline.
In a detox facility, clinicians will address the various aspects of a person’s addiction and create a customized treatment plan to help the patient get through the withdrawal timeline with minimal pain. A detox facility will address the extent of a person’s drug use, and when they last consumed drugs or alcohol. Treatment plans will also take into account if a person has attempted sobriety before, and what happened during those prior attempts. A patient’s history in regards to previous sobriety attempts will inform their current detox treatment plan.
Detox facilities are designed to get patients through the withdrawal timeline with minimal pain and to reduce the risk of severe side effects. When someone tries to quit using drugs, mental and physical symptoms of withdrawal are often debilitating. In a detox facility, clinicians can administer safe medications to address and alleviate these symptoms.
While detox programs effectively get clients through the acute phase of withdrawal, they cannot treat the underlying issues that contribute to drug addiction. For this reason, experts recommend that people participate in ongoing treatment, either in the form of inpatient or outpatient therapy, after undergoing detox. Attending a detox program is just the first step in the addiction treatment process because detox only treats physical withdrawal but does not address mental, emotional, and behavioral aspects of drug and alcohol abuse.
Detox facilities give patients access to a team of treatment specialists who are invested in helping patients get through the withdrawal timeline, and go on to maintain sobriety. Attending an inpatient detox facility can also keep patients away from harmful, outside influences that may tempt them into retaking drugs once painful withdrawal symptoms start to manifest.
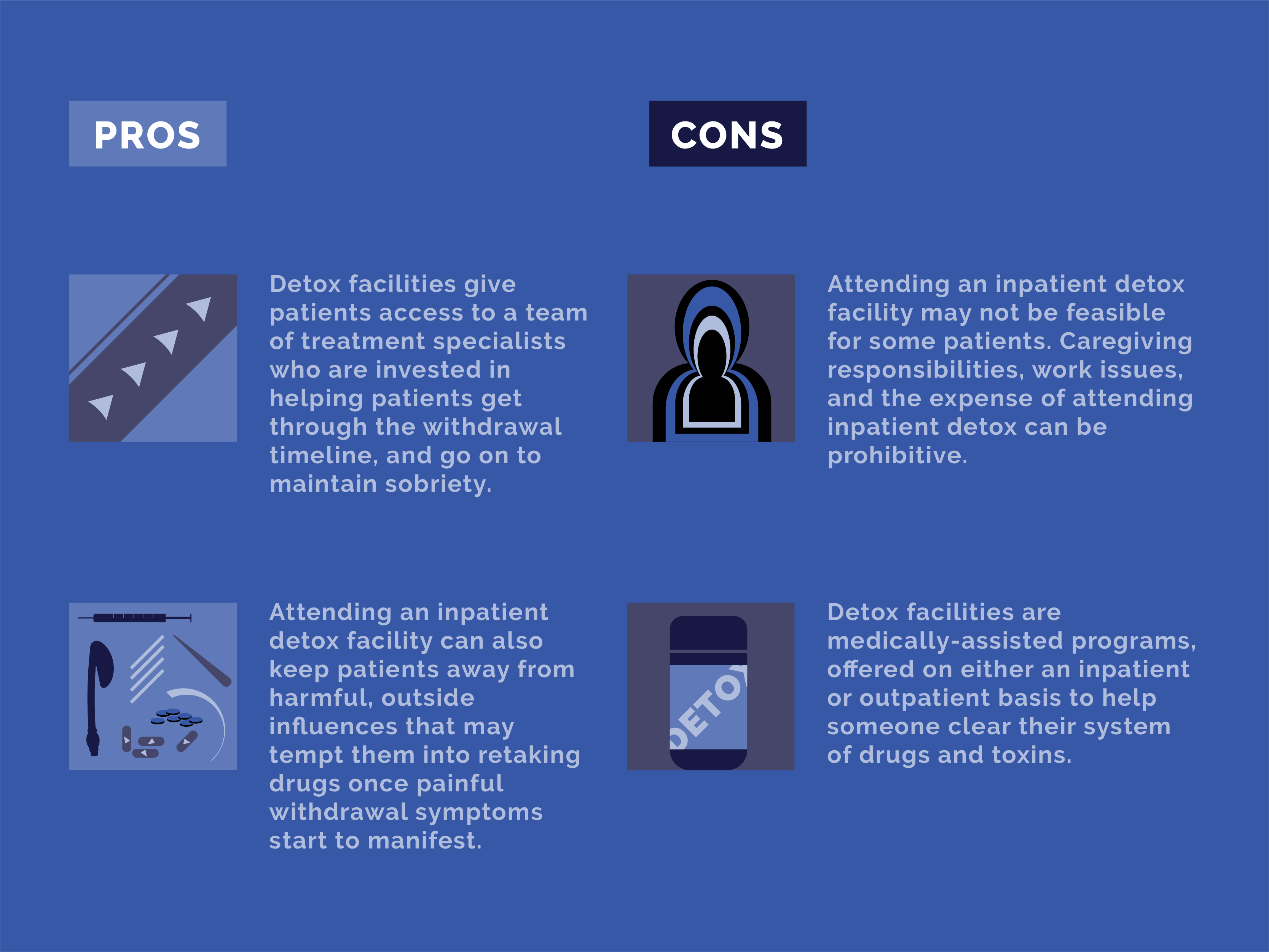
Attending an inpatient detox facility may not be feasible for some patients. Caregiving responsibilities, work issues, and the expense of attending inpatient detox can be prohibitive.
Detox facilities are medically-assisted programs, offered on either an inpatient or outpatient basis to help someone clear their system of drugs and toxins. These facilities are staffed with doctors and nurses, and patients can be given medications to help them through the withdrawal timeline.
Detox is necessary for drug and alcohol addiction, and the severity of a person’s addiction will determine how long they will need to attend a detox facility. For example, detox from severe alcohol addiction can be incredibly dangerous. For these patients, they will need to stay onsite while they overcome acute withdrawals. Patients who are also struggling with suicidal ideations, panic attacks, or other severe mental health disorder symptoms will have access to doctors and professionals who can assist them with these issues while they detox from drugs or alcohol in a safe, secure medical setting.
Individual psychologists can counsel people with emotional issues, mental health disorders, or patients with substance use disorder. Individuals who are going through distressing situations can also benefit from meeting with a psychologist one-on-one.
The duration and timeframe of attending individual counseling sessions with a psychologist can vary significantly for each patient. For some, they may only need to attend counseling for a brief period that coincides with a traumatic, stressful event or transition in a person’s life. In other cases, people may need to attend counseling for weeks, months, and sometimes years.
A psychologist can have different levels of education and credentials. Ph.D. psychologists typically go through five years of graduate training in their field. PsyD psychologists possess the same level of training as Ph.D. psychologists, but their training places less of an emphasis on experimental methods and research. To be fully licensed to practice psychology, graduates must complete at least two years of supervised experience in their state.
Psychologists can have their own individual practices, be a part of a group, or practice out of a hospital or other clinical setting.
Psychologists can address a range of subjects and concerns their clients may have. They can help patients work through short-term problems such as grief or job loss. Patients with complicated emotional issues or trauma from a past event can benefit from speaking to a licensed psychologist. Patients with mental health disorders, or drug addiction issues can also find it helpful to attend sessions with a psychologist who can address their needs.
Psychologists can offer patients support and encouragement, and also create treatment plans that take into account a patient’s needs, concerns, history, characteristics, and values.
When a patient can build a good working relationship with a licensed psychologist, they can gain valuable insight into their issues and how to work through them in healthy, positive ways. Psychologists can also give patients tools to help them endure adversity or stressful events without turning to maladaptive coping mechanisms such as drug or alcohol abuse.
In most states, a licensed psychologist cannot prescribe medications to patients. For patients with more complex medical issues, they may also need the assistance of a psychiatrist, who specializes in prescribing medications and monitoring their effects on the patient’s overall health and well-being.
Attending counseling or therapy one-on-one with a licensed psychologist is incredibly beneficial for people who struggle with complex emotional issues, pain, and trauma. For people who are addicted to drugs and alcohol and also have a co-occurring mental health condition, attending counseling one-on-one with a licensed psychologist is crucial to the recovery process.
Experienced psychologists are trained and knowledgeable on how to approach treatment methods for patients with a dual diagnosis. A psychologist will primarily focus on talk therapy methods that are designed to assist patients with emotional suffering related to their diagnosis. Psychologists can offer patients coping mechanisms and practical techniques for how to change behavioral issues and addictive impulses.
A psychiatrist can assist people with mental health disorders and complex emotional issues that require prescription medication.
The number of times a person may need to see a psychiatrist can vary significantly based on their medical needs. For people with severe mental health disorders, having long-term or even lifelong support from a psychiatrist is essential for them to maintain good mental and physical health.
A psychiatrist is a medical doctor who has completed medical school and a residency program in a psychiatric facility or care unit. Psychiatrists specialize in diagnosing and treating mental health disorders, and also prescribing medications to patients. A board-certified psychiatrist has passed a written and oral exam after graduating and completing residency.
A psychiatrist can work in a range of settings and clinical practices. They may work in a psychiatric hospital, university medical center, as part of the judicial system, or in nursing homes or rehab programs. Some psychiatrists may even have their own private clinical practice.
Patients with suspected and diagnosed mental health disorders can benefit from seeing a psychiatrist.
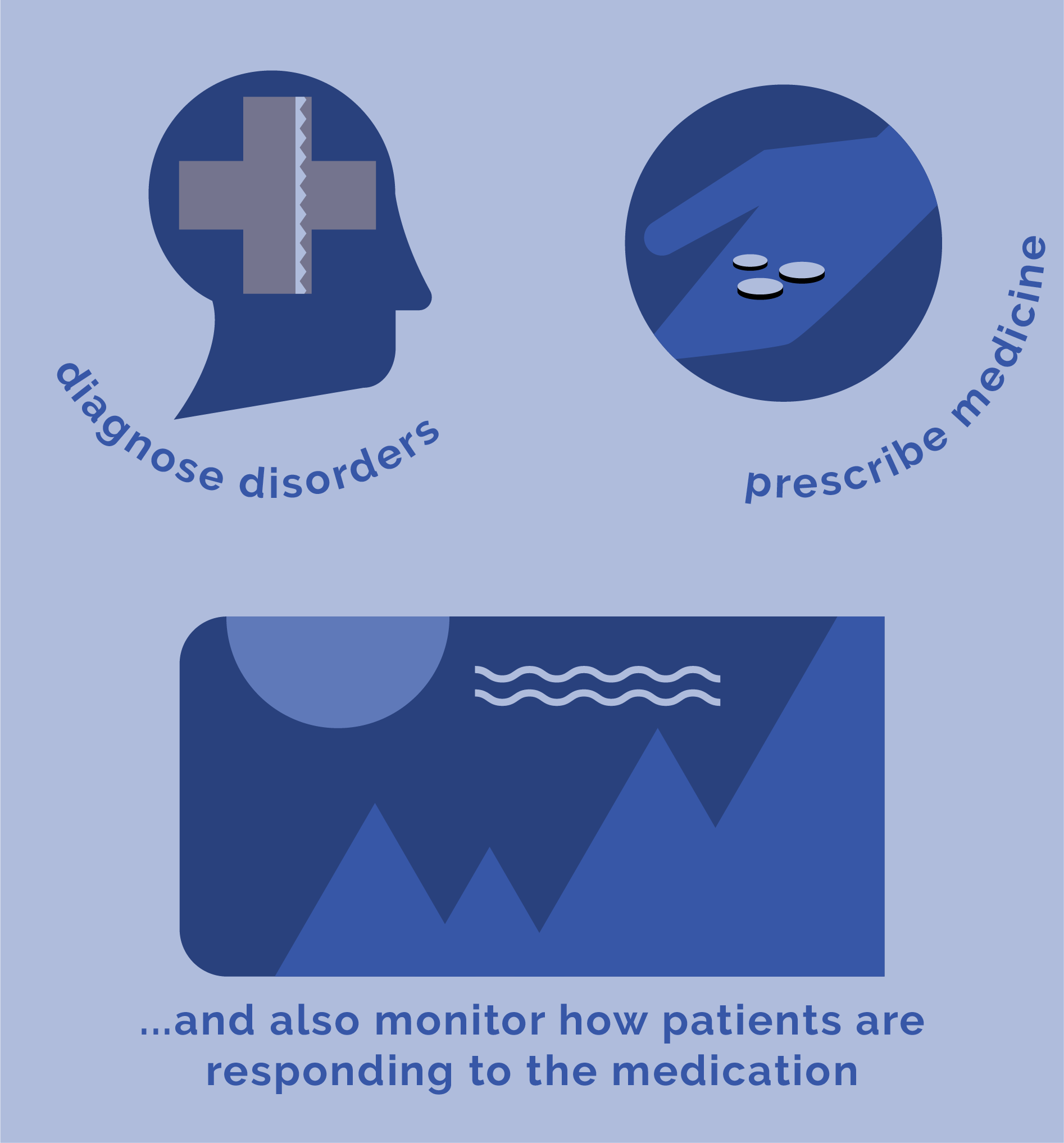
Psychiatrists can diagnose mental health disorders, prescribe medicines, and also monitor how patients are responding to the medication. Mental health medicines can interfere significantly with other prescriptions, supplements, and OTC medications. A psychiatrist specializes in how these different drugs impact each other, and they can adjust a patient’s medication, or change their prescription.
People with distressing mental health disorder symptoms can significantly benefit from seeing a psychiatrist since these professionals are knowledgeable, licensed, and experienced with how medications can alleviate symptoms and distress.
Psychiatrists do not offer counseling or therapy. For most mental health disorder patients, medication alone is not enough to address all of their symptoms. Medication won’t help patients develop the coping mechanisms they may need to avoid triggers and other harmful influences. Patients are better suited to using a variety of services for their condition, including psychiatry and counseling.
A psychiatrist focuses more on medication management and using pharmaceuticals to give their patients relief from symptoms. Psychiatrists can also diagnose mental health conditions and behavioral disorders, and prescribe tests and other diagnostics to rule out physical health problems that may be mimicking a mental health disorder, and vice versa.
Psychiatrists also monitor the effects that a mental health condition can have on physical health problems. They can also track how medications for mental health may impact medicines a person takes for physical health conditions. For patients who are dealing with severe mental health conditions, medications are critical for recovery. In many cases, people with a dual diagnosis will need care from a team of medical professionals, including psychiatrists, psychologists, their primary care physician, and other counselors and social workers.
Peer support specialists help people who have been diagnosed with a mental health disorder.
Patients can speak to and meet with a peer specialist for weeks or months.
To become certified as a peer specialist, a person will need to have been diagnosed with a mental health condition, have used mental health services in the past or is currently using mental health services. They will need to complete a four-hour training course and pass a written exam to become a peer specialist. To continue serving the community in this capacity, a certified peer specialist will need to earn at least twenty continuing education credits every two years. Certification credentials may vary somewhat depending on which state a person will practice in.
Peer specialists work in public and private settings. They may offer support in an inpatient care facility, or through community-based services.
Peer support specialists can’t diagnose patients, prescribe medications, or offer specialized therapy treatments such as cognitive-behavioral therapy. A peer specialist provides support and encouragement for people diagnosed with a mental health condition.
Certified peer specialists can assist patients with creating plans for recovery and help them learn and practice new skills. Peer specialists can also help patients monitor their progress for treatment, and also show patients self-help strategies and coping techniques that a peer specialist knows first-hand.

For many patients, speaking and working with someone who has personal experience of mental health disorders is enough to encourage them to seek and maintain their treatment regimen. Peer support specialists can show patients how to cope with distress and offer the type of encouragement that a clinician may not be able to give patients.
Peer support specialists can’t diagnose a mental health condition or treat a mental health disorder with medication.
Support, encouragement, and the chance to form strong and healthy relationships is critical to recovering from a severe, dual diagnosis or mental health disorder. A peer specialist is someone who has had first-hand, personal experience with a mental health condition, or a traumatic experience that may have triggered mental illness symptoms.
These individuals are regular, everyday people who may or may not have a license to practice medicine. Instead, each state in the U.S. has different training requirements that a person must go through to become a peer specialist. Peer specialists get to share their personal experiences and the tools they’ve used to change their lives with people who are going through similar struggles. For patients, forming a relationship with a peer specialist can significantly impact their recovery.
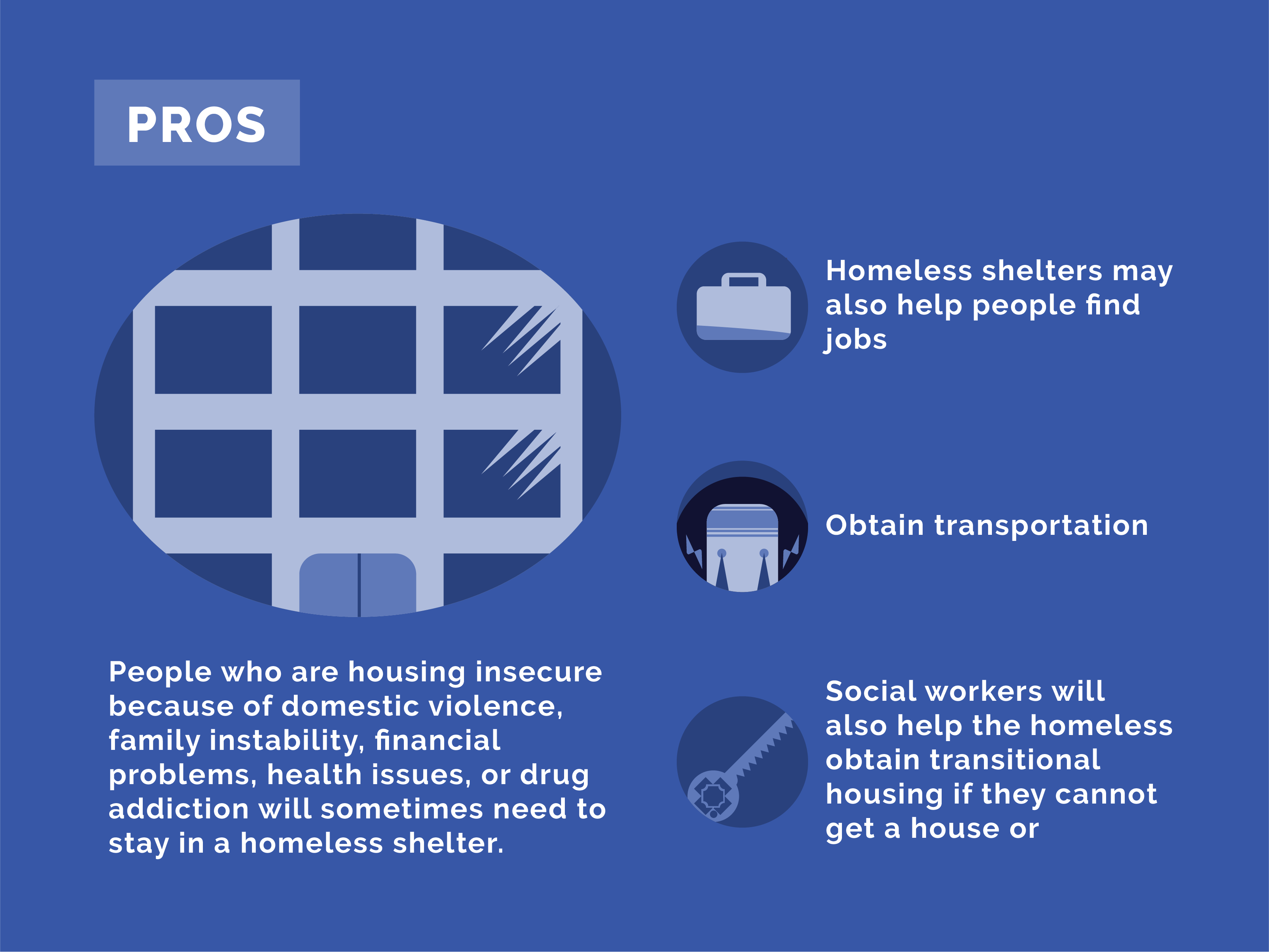
People who are housing insecure because of domestic violence, family instability, financial problems, health issues, or drug addiction will sometimes need to stay in a homeless shelter.
The amount of time a person will stay in a homeless shelter will significantly vary depending on the shelter’s capacity. Very crowded shelters may only be able to offer assistance for three to five days. Most people will stay in a homeless shelter for up to 30 days, after which, staff usually reviews the person’s case.
Licensed social workers typically run a homeless shelter. Volunteers, counselors, and therapists may also work at a homeless shelter.
Most homeless shelters are located in urban areas.
A homeless shelter will offer housing insecure people in the community shelter for a period until they can obtain safe and secure housing.
Homeless shelters offer a place for people to sleep, meals, and they may also help people find jobs, or obtain transportation. Social workers will also help the homeless obtain transitional housing if they cannot get a house or apartment on their own.

For many people, living on the street or in an abusive situation is incredibly dangerous. Homeless shelters offer vulnerable members of the community a safe place to live and assistance with how to obtain secure housing. Staying in a homeless shelter can also put an individual in-touch with social workers who can refer them to mental health services or drug rehab services.
Staying in a homeless shelter can be stigmatizing and restrictive for many individuals. Social workers and staff will do their best to keep the residents safe, but overcrowding can lead to some individuals becoming violent with other residents. Overcrowding can also expose people to poor sanitary conditions.
Homeless shelters or homeless service agencies are organizations designed to offer temporary housing for housing insecure persons in a community. These shelters exist to provide people with safety from the elements, and protection from the violence that can happen to them if they live on the street. Shelters also exist to keep other residents of a community safe.
Unfortunately, homeless shelters are often crowded and are unequipped to handle the needs of people with addiction and mental health disorders. Homeless shelter employees can refer residents to treatment programs, or mental health facilities, but the homeless shelter itself is not designed for detox, withdrawal, and psychiatric counseling.
Battered women shelters offer safe, temporary housing for abused women and their children.
Battered women shelters are similar to a homeless shelter, in that people will typically stay for about three to five days until they can secure housing. Some will need to stay for up to a month, after which a caseworker will evaluate the resident’s situation.
Battered women shelters are typically run by a team of social workers, caseworkers, and volunteers from the community.
Because women who enter a shelter are often the victims of severe mental and sometimes physical abuse and threats, battered women shelter locations are not publicized, and their locations are kept secret.
Battered women shelters address resident’s needs for secure housing, possible custody issues if children are involved, and how to safely extricate oneself from a potentially dangerous situation with an abusive partner. Shelters will also help women secure safe housing and may also offer job leads, career counseling, and transportation assistance.
Social workers at battered women shelters can refer residents to counselors and therapists who specialize in treating the victims of domestic violence.
For women and children who are the victims of domestic abuse, a battered women shelter offers a safe place to stay until they can secure permanent housing.
Battered women shelters experience similar issues like homeless shelters. They can be restrictive and may not be able to address a resident’s complex needs. Also, overcrowding can lead to potentially dangerous and unsanitary conditions.
Every day, more than 20,000 calls are placed to domestic abuse hotlines. Approximately one in four women will be abused or stalked by an intimate partner at some point in their lives. Unfortunately, women are at higher risk than men of becoming homeless due to domestic violence or abuse at the hands of a family member or intimate partner. Women also face unique obstacles that make them more likely to face housing insecurity. Pregnancy and childcare responsibilities make it more challenging for a woman to earn a living that can keep her and her children securely housed in a safe place. Women are also more likely than men to experience physical health problems and mental health disorders that can increase their likelihood of becoming addicted to drugs or alcohol and losing their home.
A battered women’s shelter is designed to keep women and any children they may have safe from a violent family member or intimate partner. These shelters are often overcrowded and struggle with having enough supplies for the residents. Shelters are also designed to refer women to mental health professionals, rehab centers, and also help her find a job, childcare, and a safe place to live.
A court-ordered program is for people who have had run-ins with the criminal justice system because of an addiction issue.

Most court-ordered rehab programs last for thirty, sixty, or ninety days.
Rehabilitation facilities that serve court-ordered offenders are licensed through the state in which they are located.
Rehab programs can be located in a variety of settings. They may be part of a hospital or clinic or take the form of a separate facility.
Instead of going to jail, a judge may order an arrestee to attend a substance abuse program. With a court-ordered program, a person’s substance abuse issues are addressed directly in the hopes of rehabilitation and stopping the individual from committing future crimes related to drug abuse.
Court-ordered programs typically require the defendant to attend an inpatient rehab and detox program. Arrestees can attend counseling and therapy with professionals who specialize in drug addiction issues and how they can influence someone to commit a crime.
For many defendants, attending a court-ordered program instead of going to jail can help them achieve sobriety. It is less stigmatizing for the individual and their family. Court-ordered programs also help the defendant and their loved ones directly and prevent further victimization if the person were to be sentenced to jail.
Although attending a court-ordered rehab program can help someone achieve sobriety, for most drug or alcohol addicts, outside pressure to get clean is often not enough. Most people need to want to personally get clean from drugs to achieve and maintain initial sobriety.
Around a quarter of all jail and prison inmates claim that they committed their crime to obtain money for drugs. Unfortunately, drug addiction completely changes the way a person thinks, feels, and behaves. The brain’s complex risk and reward circuitry are changed when someone becomes addicted to a substance, and they will become preoccupied with how to obtain drugs, and how to get high. This can often lead to an increase in legal issues and crime.
Attending a substance abuse facility can put an arrested person in contact with mental health professionals, who can begin to treat underlying mental health conditions that are contributing to a person’s addiction and criminal behaviors. It’s true that a person can’t be forced to recover from addiction, but being exposed to addiction specialists and other doctors can put an at-risk person on the path to sobriety and help them find relief from mental health disorder symptoms, and keep them out of jail.
12-step meetings can serve a variety of people in the community. There are dozens of different 12-step meeting programs that address specific issues, such as alcohol addiction recovery, recovery from narcotics abuse, or gambling. People who are in recovery for addiction and loved ones of addicts can benefit from attending a 12-step meeting program.
A 12-step meeting lasts about one hour. People can attend as many meetings as they like, and 12-step meetings can be held in a single location for years on end.
Therapists, social workers, and former addicts often lead a 12-step meeting. Members are encouraged to speak and share throughout the sessions.
A 12-step meeting can occur in a variety of settings. They may be held in a church, a leader’s home, or in a clinical setting.
12-step meetings can address a variety of topics for members. The most popular type of 12-step meeting is AA or Alcoholics Anonymous. But, 12-step meeting programs can address other types of addiction, such as Narcotics Anonymous, or Gamblers Anonymous
12-step meetings are designed to encourage and support people in recovery from addiction. The meetings center around the idea of the “12-steps,” which is a blueprint for how to live a sober life and avoid relapse. During a 12-step session, members who are struggling with cravings and relapse are encouraged to share so the group can offer their support.
For many people in recovery, recovering from an addiction is an isolating experience, and cravings for substances or addictive activities can be intense during periods of high stress. 12-step meetings can give people in recovery the encouragement they need to stay clean.
These groups do not offer medical support or intensive one-on-one treatment. People with an active addiction and people with mental health disorders can’t use a 12-step program to replace actual medical care.
12-step meetings or 12-step programs are support groups that are typically used as a form of aftercare treatment, where patients can voluntarily participate in the sessions after obtaining initial sobriety. Some 12-step meetings are also designed to help the family members and loved ones of people with substance use disorders, behavioral addictions, and mental health issues.
These programs place a heavy emphasis on spirituality and personal accountability, and how they can be used to help someone overcome an addiction or other profound struggles. The programs aren’t focused solely on one particular religion, and even non-religious people can benefit from these meetings. They offer people a chance to share their struggles and their victories, and attendees do not have to speak or share anything if they are not ready.
12-step programs center around the idea of voluntary disclosure, which can be helpful and therapeutic for members. 12-step meetings also give participants a chance to form strong friendships with people in similar situations. These programs often start with the addiction or behavioral issues they address, and end with the word “anonymous.” Participants’ identities are protected, and they do not have to share their names or any other identifying information in the group.
AA is a 12-step program designed specifically for people in recovery from alcohol addiction and their loved ones.
AA meetings last about one hour, and members can attend as many meetings as they like for as long as they need. Leaders will try to ensure that meetings do not go over an hour so that people with busy schedules can still attend.
In most cases, former alcoholics will lead AA meetings. Sometimes, a meeting will have a key speaker scheduled to share important insights into recovery from alcoholism.
An AA meeting can be held in a variety of locations. Typically, AA meetings take place in churches or community centers.
AA is designed to encourage recovering addicts to stay sober and avoid relapse.
People attend AA meetings for encouragement to stay sober, and support for their struggles from people with first-hand experience of alcoholism.
These meetings can help a person struggling with cravings to use alcohol from relapsing. They can also offer support and encouragement to loved ones of recovering addicts. Attending an AA meeting can help those in recovery feel less alone in their journey to maintain sobriety.
AA meetings are not designed to offer treatment or medical advice.
Alcoholics Anonymous is a worldwide organization, with more than 100,000 groups across the globe. A.A. meetings center around spirituality and spiritual practices to help members achieve sobriety and remain abstinent from alcohol.
Narcotics Anonymous is a 12-step program that addresses the needs of those in recovery from narcotics addiction.

An NA meeting lasts about one hour.
Most NA meeting leaders are former addicts themselves, but sometimes a social worker will lead NA meetings.
NA meetings don’t offer medical treatment or advice, so locations for NA meetings are flexible. Leaders can hold meetings in their home, and churches and community centers may also hold NA meetings.
An NA meeting will address the problems associated with recovery from addiction to narcotics and are designed to help patients avoid relapse.
Members are encouraged to share their experiences and struggles related to their recovery from narcotics addiction so the group can offer their support.
Recovering from addiction can be an isolating experience. For many recovering addicts, the struggle to maintain sobriety is difficult without outside support. NA aims to bridge some of the gaps between rehab and maintaining sober living outside of a facility.
NA meetings are not intended to replace medical care, and they do not offer members medical advice.
Narcotics anonymous is another 12-step program that is designed to help people maintain sobriety from narcotics. Former addicts typically lead the agenda and focus on using spirituality and personal accountability to remain abstinent from narcotics. Like A.A., NA is not affiliated with any one specific group. Instead, it is a non-profit fellowship.
While a group like N.A. cannot give a person treatment for a mental health disorder, it can help them remain sober. Abusing drugs like narcotics can worsen mental health disorder symptoms, and it’s critical that people in recovery from substance abuse can maintain their sobriety. N.A. operates under the principle of voluntary disclosure and offers participants a chance to share their experiences, hopes, and concerns with people going through similar issues.
GA is for people in recovery from gambling addiction.
A GA meeting will last about one hour, and leaders will do their best to limit the meeting to that timeframe. Limiting sessions to a predictable one-hour timeline can help encourage people to attend if they have busy or hectic schedules.
GA leaders are usually former addicts.
These meetings can take place in a leader’s home, religious institution, or community center.
Issues related to relapse and maintaining sobriety from gambling are addressed during a GA meeting.
GA meetings are intended to offer members encouragement and support.
GA meetings can help individuals maintain their sobriety with support from people with first-hand experience of these struggles.
Like all 12-step meeting programs, GA is not intended to give medical advice, or replace necessary medical treatment.
G.A. is very similar to both A.A. and N.A., but the meetings are geared toward helping people abstain from gambling. Gambling is considered a behavioral disorder, and the symptoms of gambling addiction, and how people withdrawal from gambling addiction are very different than the withdrawal process involved in drug or substance abuse addictions. The only requirement to join a G.A. support group is to have a desire to get better and abstain from gambling. Members do not have to identify themselves or speak during a meeting.
As is the case with other anonymous support groups, G.A. is not a replacement for medical care for mental health disorders. Instead, GA offers participants the chance to share their wisdom, experiences, and concerns with a group of people who know first-hand what it’s like to live with and overcome a behavioral addiction.
Pain management clinics are for people suffering from chronic, debilitating pain.
Chronic pain is a lifelong issue, and patients will often need the services of a pain management clinic or specialist for the rest of their lives. Patients with acute pain issues may only need treatment for several weeks to months until they heal from their injuries or disorder.
Pain management clinics are staffed with licensed doctors and nurses who specialize in the management of chronic and acute pain.
Pain management clinics can be located in a hospital setting or as private practices.
Doctors and nurses at a pain management clinic specialize in treating both chronic and acute pain. Treatment plans are customized to the individual patient’s needs, lifestyle, and goals for treatment.
A pain management clinic’s purpose is to offer the patient’s symptom relief and a safe and effective way to manage their pain syndrome. Doctors may use a combination of different treatments and therapies, including prescription medications, physical therapy, steroid injections, and nerve blocks. Physicians may also prescribe massage therapy as a treatment for pain.
For patients with chronic pain conditions, pain management clinics offer a range of services that are specifically designed to help people with these issues.
Pain management clinics do not always offer uniform care. What one clinic offers and recommends may not be recommended at another clinic. Patients may need to shop around to find a clinic that suits their needs and prior medical history.
People who’ve been diagnosed with substance use disorder and a physical health issue that causes acute or chronic pain, may or may not be able to take strong prescription painkillers. Unfortunately, medical science has not advanced very far when it comes to treating chronic pain. Most of the popular and effective pain medications used today are incredibly addictive. If a person with addiction issues is prescribed an addictive painkiller, this can quickly derail their progress towards sobriety. Also, people with untreated mental health disorders are at higher risk of becoming addicted to painkillers than the general population. For pain patients with these unique needs, a pain management clinic will typically prescribe non-addictive narcotic painkillers.
Because of the opioid crisis, many pain management doctors are speaking out against their colleagues who prescribe addictive opioid medications. Fortunately, it is possible for patients with a dual diagnosis and chronic pain to find non-addictive medicines for treating their pain without risking setbacks in their road to recovery from addiction.
Churches and religious institutions can offer support for community members of faith that are struggling with mental health disorders and drug addiction. Religious communities can also assist family members of mental health disorder patients and people with addiction problems.
Church and worship services will vary significantly depending on what faith the institution subscribes to. Most worship services will last for one hour, or sometimes for several hours. Religious holidays and certain ceremonies can influence the duration of a worship service.
Religious institutions are led by licensed and certified religious leaders and clergy.
Churches and other religious institutions are located throughout a variety of urban, rural, and suburban neighborhoods. There are even online churches, and religious communities that people can join that are location independent.
Faith communities can offer support and encouragement for families that are struggling with mental health and addiction issues.
Religious institutions frequently offer their members faith-based support groups for substance abuse and mental health disorders.
Believing in a higher power and having faith can help people maintain sobriety and get through adverse and stressful times. Attending church or other religious institutions gives members access to other people who share their faith and are willing to support them during their time of need.
Attending church or other religious institutions are not meant to replace necessary medical care. Churches are not licensed to offer medical treatment.
Strong and supportive relationships are critical to helping someone recover from a mental health condition or achieving and maintaining their sobriety. Church support groups can offer members the chance to hear testimonies from people who’ve recovered and also give members a chance to listen to sermons or other speeches that destigmatize the condition and view the whole person as someone worthy of friendship and love. While the church can address the spiritual aspects of a patient and their need for community, it can’t offer medical treatment.
Marriage and family therapy is designed to meet the specific, emotional needs of married couples and their children or extended family members.
Usually, marriage and family therapy is goal-oriented, and people attend sessions for a set period. They may attend once a week for several months, or up to a year in some cases.
A licensed marriage and family therapist is a trained mental health professional who can diagnose and treat mental health disorders. MFTs are not authorized to diagnose mental health conditions, but they can offer beneficial talk therapy for families in crisis.
Marriage and family therapy sessions are typically located in private, clinical practices. MFTs may also practice in community centers, hospitals, outpatient mental health services, or in substance abuse programs.
A marriage and family therapist will address specific, adverse issues affecting a married couple or extended family. Sessions are usually goal-oriented and designed to improve communication between the family members.
Marriage and family therapists offer guidance to their patients who are struggling with mental health or substance abuse issues.
This type of therapy is usually brief and goal-oriented. Families struggling with a specific issue can most benefit from marriage and family therapy.
Marriage and family therapy is not suited for complex or ongoing issues. People with mental health disorders or substance use disorder typically need integrated treatment models that utilize a variety of treatment methods to make a full recovery.
Licensed marriage and family therapists and MFTs are trained mental health professionals who are experienced with psychotherapy practices and the impact that dual diagnosis can have on families. MFTs who are licensed can diagnose and treat mental and emotional disorders, and the way they harm family systems.
Marriage and family therapy is typically brief, and the sessions focus on reaching a specific goal for the family, such as improving the marital relationship, a person’s ability to communicate, or how to decrease the impact of dual diagnosis on a child’s development. Most family and marriage therapy programs are completed successfully within fifty sessions. For people with a dual diagnosis who are married or have children, family, and marriage therapy is incredibly beneficial to helping them maintain and strengthen their intimate relationships.
CSWs offer assistance to members of the community who are struggling with mental health and substance use disorders.
A clinical social worker often works with patients for weeks, months, or years while treatment is ongoing.
A licensed clinical social worker must complete a Master of Social Work degree from an accredited school. They may also have to complete several years of additional supervised clinical experience and pass an exam. Licensing and renewal requirements will vary depending on the state in which a CSW wishes to work.
CSWs will counsel patients in a variety of different settings. A clinical social worker may be employed in a hospital, a government agency, or community service.
Clinical social workers will address several areas of a person’s life where mental health or substance abuse issues are impacting them. A CSWs goal is to accurately assess the individual’s current condition, their goals for treatment, and how to reduce the risk of harm to the patient.
Patients with a clinical social worker assigned to their case may be offered counseling from a clinical social worker directly. CSWs often give valuable insight to doctors and other healthcare workers regarding a patient’s treatment plan and what they need to recover.
Patients can benefit from a CSW’s expertise and experience in the field, and their input into case management and treatment plans.
While clinical social workers can sometimes offer counseling services for individuals and their families, they are not medical doctors. CSWs often have large caseloads and may not be able to give patients as much attention as their case warrants.
Outpatient treatment programs offer specialized care for people with mental health and substance use disorders.
The amount of time a patient may need to attend outpatient care can vary significantly. The extent of their condition and prognosis for recovery will all influence the outpatient treatment timeline.
According to the National Institute on Drug Abuse (NIDA), patients need to remain in treatment for a sufficient length of time for it to be effective. Most of the time, people need to remain in treatment for at least three months to be successful.
The weekly time commitment for outpatient treatment also varies depending upon a person’s needs. Some people may be able to participate in standard outpatient services, which involves spending fewer than nine hours per week in treatment for adults and fewer than six hours weekly for adolescents.
An outpatient treatment program is subject to state licensing requirements.
Outpatient treatment is typically offered to patients in a hospital or clinical settings. Sometimes, community organizations or government organizations will provide outpatient treatment.
Outpatient treatment programs can address the mental health and drug addiction needs of their patients.
Healthcare and addiction specialists in an outpatient treatment program will offer patients a variety of services, dependent on their needs and circumstances. Patients may attend group, family, and one-on-one therapy. Outpatient treatment may offer medical detox options as well. Group and recreational activities may also be a part of a program.
Outpatient treatment programs are often flexible and allow patients to get the care they need without having to stay overnight in an inpatient facility. This will enable them to continue working, going to school, or caring for minor children or other family members.
Outpatient treatment programs are not intensive enough for people with severe addictions or mental health disorders.
Outpatient programs allow patients to live away from a treatment facility, but they must return to the facility for pre-scheduled therapy sessions or other treatment programs during the day. The patient’s specific needs will determine how long they need to attend outpatient treatment and how intense or structured an outpatient program needs to be to help them recover. In most cases, patients participate in outpatient treatment for a few hours every weekday for several months.
Inpatient treatment programs are designed to address the healthcare needs of people with severe addiction and mental health disorders.
In most cases, a person will attend inpatient rehab for thirty days, sixty days, or ninety days. Rarely will treatment exceed these durations, but in some cases, it may be warranted.
An inpatient treatment facility must be licensed in the state it is located.
Inpatient treatment programs take place inside a hospital.
Severe drug addiction and mental health disorders are addressed in an inpatient facility.
Patients usually undergo a medically supervised detox as the first step for drug addiction issues. Inpatient treatment allows patients to recover from their disorder in a safe, secure setting that is designed specifically for their needs. Patients will attend a combination of different therapies and group support meetings. They’ll have access to a team of doctors, nurses, therapists, and benefit from the comfort of their peers.
Inpatient treatment centers are secure and offer comprehensive treatment regimens. Detoxing from drugs, and recovering from an addiction or mental health crisis in a safe environment gives patients the chance to focus on their recovery, free from harmful outside influences.
Inpatient treatment may not be feasible for patients with caregiving responsibilities. Patients may also fear losing their job if they were to attend an inpatient program.
Unlike outpatient treatment programs, an inpatient treatment program requires the individual to reside onsite in a hospital setting. These programs typically run for either thirty days, sixty days, or ninety-day durations. For some patients, they may need to attend inpatient treatment for longer than 90 days.
Patients with severe addiction and mental health disorders can significantly benefit from inpatient treatment. They are kept safe, surrounded by medical professionals 24/7, and inpatient treatments offer patients a drug-free environment, which substantially decreases the chance of relapse. Staying in a treatment facility that is located in a hospital allows patients to go through medically-assisted detox, and also obtain comprehensive mental health treatment from a team of psychologists and psychiatrists who work at the hospital.
A residential treatment program is designed to help people with substance abuse and addiction issues achieve and maintain sobriety.
Residential treatment programs typically last for a period of thirty, sixty, or ninety days. Patients may attend for a longer or shorter duration, depending on their needs.
Residential treatment programs are subject to state licensing requirements.
A residential treatment program is similar to an inpatient program, but they are usually located in facilities separate from a hospital and are generally privately owned.
Residential treatment programs address issues related to substance abuse and addiction and how to achieve and maintain sobriety.
A residential treatment program may offer medical detox services. Also, patients will also have access to a team of clinicians who specialize in treating addiction issues. Residents may attend one-on-one therapy and group or family counseling. Doctors are staffed at a center and can prescribe medications. Some residential treatment programs offer progressive therapies and recreational activities for their patients.
Patients can recover from drug abuse and addiction in a secure, tranquil environment, surrounded by doctors and staff members who specialize in handling their medical needs.
Residential programs can be cost-prohibitive for many patients. Staying in a residential program is not always feasible for some patients who have caregiving or work responsibilities, even if they could most benefit from this type of treatment model.
These programs are similar to inpatient treatment programs, in that patients are required to live onsite for a set duration. However, residential rehab programs take place in separate facilities that are designed to offer patients a home-like setting. Residential treatment programs are not administered in a hospital or clinical treatment center, and they can give patients the chance to feel more at-home, relaxed, and comfortable. For some patients, they may exit a hospital inpatient treatment program and go to a residential treatment program to continue their care before transitioning to an outpatient program, or a sober living situation.
Sober living facilities are transitional housing arrangements for people in recovery from addiction who have recently completed a stay at an inpatient or residential treatment center.

A person can stay in a sober living home for several months to a year before transitioning back into the community and independent living fully.
Sober living homes are subject to state licensing and regulation requirements.
A sober living house can be located in an urban, rural, or suburban setting.
Sober living homes address the unique problems that face people in recovery from severe addiction. These patients can significantly benefit from transitional housing after leaving an inpatient rehab program. Patients are typically not in a position to go straight from a structured, drug-free environment to “normal” life.
Social workers and clinicians in a sober living home help patients transition back into the community and regular life. They may offer residents job and financial counseling, and help them create and achieve goals for living an independent, drug, and alcohol-free life.
Patients are plugged-in to a community of like-minded individuals, and given structure and continuity of care.
Sober living may seem restrictive and stifling for some patients. Privacy can also be an issue.
Relapse is a substantial risk for people living with drug addiction issues. Relapse does not mean that initial treatment wasn’t a success. But, for many patients, relapse poses a real danger to their health and well-being. Several months after a person leaves an inpatient treatment center or residential program are when that person is most vulnerable to stress and the risk of relapse. What sober living communities aim to do is offer patients the chance to continue living in a somewhat structured, drug-free environment that also provides them help and guidance for how to transition to living outside of a treatment facility.
The VA is a part of the government responsible for providing medical care and benefits to members of the military and their families.
People who join the military and their families can receive care and benefits from the VA for life.
The Department of Veterans Affairs is an agency of the federal government.
VA offices are located throughout the U.S.
The VA is designed to meet certain needs of service members and their families. The VA is most known for the healthcare services they offer to both veterans and active-duty military. Spouses of military veterans may also receive benefits from the VA.
Service members and their families can receive both physical and mental healthcare through the VA. The VA also offers cemetery services for military members. Service members can also receive other benefits through the agency, including college and homeownership assistance.
For service members, the VA may be their only source of guaranteed care for mental health and substance use issues. Benefits and healthcare through the VA are guaranteed for service members.
The VA has come under recent scrutiny regarding their assessments for risk and healthcare outcomes. As one of the largest healthcare providers in the country, the VA is often overwhelmed with demand for services, and military members who live in rural areas may be subject to long wait times for much-needed care.
Nursing homes are designed as long-term care and living facilities for senior citizens.
A patient who enters a nursing home will typically live there for the rest of their lives. Some patients may live in a nursing home for decades.
Nursing homes are subject to strict state licensing and regulation requirements. Nursing homes are periodically inspected for compliance with these regulations.
Nursing homes are located throughout the U.S. in a variety of urban, rural, and suburban settings.
A nursing home mainly addresses aspects of safety. Many elderly individuals can’t live at home or otherwise age-in-place. Family and friends may not have the skills or finances to care for their elderly loved ones, especially if they have significant mental health and physical needs. A nursing home keeps elderly patients safe and offers them 24/7 access to healthcare workers. Nursing homes also give elderly residents the chance to socialize with their peers.
Residents will be assigned either a shared or private room. Nurses and doctors will monitor and administer their medication and also give patients personal care and assistance. Residents will also enjoy social and recreational activities.
For some patients, living in a nursing home is ideal. It offers safety, security, and 24/7 personal and emergency care. The social aspects of a nursing home can also benefit elderly patients.
Nursing homes can be restrictive for some people, especially if they are used to independent living. Patients may become homesick or depressed at the sudden change.
Millions of seniors struggle with drug or alcohol abuse. When most people hear the word “addiction,” they typically don’t picture an older person abusing drugs or alcohol. But the elderly face certain obstacles and other challenges related to the aging process that can make them particularly vulnerable to addiction or mental health problems.
Losing loved ones, and dealing with chronic pain conditions or other physical health issues can trigger depression and anxiety. Seniors are also more likely to experience depression and sleep disorders than younger people, which can trigger substance abuse, too. The elderly are also prescribed medications for managing many diseases related to aging that can be addictive.
Retirement communities are designed to meet the specific needs of senior citizens, including mental health care and addiction issues. Nursing homes also offer seniors round-the-clock care. For some seniors, aging-in-place at home can be isolating and lonely, and contribute to mental health conditions or alcohol and drug abuse. Nursing homes and retirement communities for the elderly give seniors the chance to socialize and bond with other residents and nursing home staff. Long-term care facilities also have medical staff on site to assist senior patients with both physical and mental health issues.
Partial hospitalization programs are designed to address the unique needs of people with addiction issues. Unlike an inpatient or residential program, a PHP allows patients to attend treatment programs in a hospital setting for several hours per day during weekdays.
Partial hospitalization is the most intensive form of outpatient care. This level of care usually offers at least 20 hours of service per week. People in partial hospitalization typically spend several hours most days of the week in treatment, but they return home at night. Partial hospitalization can serve the needs of those who have a more severe addiction but do not require around-the-clock care.
PHPs are subject to state regulations and licensing requirements.
A PHP takes place in a hospital or clinical setting.
PHP programs address the needs of patients who are leaving a residential rehab or inpatient program. Patients who are going through relapse may also benefit from a PHP program, depending on the severity of their issue.
Patients in a PHP program are given focused, intensive counseling, and therapy. They may also need medical treatment for detox and withdrawal symptoms.
PHPs are more cost-effective than inpatient or residential treatment programs, and usually address the same issues as these programs.
PHPs can be restrictive and may not offer enough flexibility for patients with school, work, or family responsibilities.
Every dual diagnosis patient is different, and not everyone will require intensive treatment to manage mental health symptoms and achieve sobriety. But dealing with withdrawal and detox symptoms along with a mental health disorder can be debilitating for some patients. Partial hospitalization is also called inpatient hospitalization, and patients can detox and also receive care for a mental health disorder in a hospital setting. This type of treatment program is incredibly helpful for patients with severe addiction and mental health issues. Detoxing in a hospital can keep patients safe and secure and also give swift medical attention for painful, possibly dangerous withdrawal symptoms, and severe mental health issues such as psychosis or suicide attempts.
Community mental health centers offer care and services for people in a local community who’ve been diagnosed with a mental health condition.
People can use the services of a community mental health center for many years.
These facilities are subject to state licensing regulations.
Community mental health centers are located in cities and small towns throughout the U.S.
These facilities address mental health treatment and ongoing care and maintenance for mental health patients and their loved ones.
A community mental health facility will offer care and counseling either in the facility itself or in the patient’s home.
Community mental health centers offer a continuation of care for people with a mental health diagnosis. Continuity of care is critical for preventing a relapse of symptoms, or addressing symptoms quickly should they arise. These facilities can also refer patients and their families referrals to other doctors who can help treat a variety of issues related to a mental health diagnosis.
Community mental health centers aren’t always equipped to handle severe cases of mental illness. Caseworkers may be overwhelmed with work, and unable to give their client’s attention they may need.
Addiction and mental health disorders are chronic, lifelong conditions. Although they are unfairly stigmatized, they are similar to other chronic physical conditions such as diabetes and heart disease. Mental health and addiction patients need ongoing care and maintenance, just like a heart disease patient, and they also need access to a team of medical professionals who can help them adequately manage a complex dual diagnosis.
Community health centers are non-profit, consumer-directed health care facilities that offer patients access to comprehensive primary and preventative medical and mental healthcare. A community health center is usually part of a network of non-profit health facilities that are staffed by medical doctors, mental health counselors, social workers, and nurses. People who complete rehab will typically need to access a community health center to find resources and healthcare facilities that can service their needs and help them avoid a relapse of addiction or mental health disorder symptoms.
Telemental health services are for patients with mental health issues, substance use disorder, and behavioral problems.
The length of care will depend on what type of services a patient needs.
Licensed psychiatrists, psychologists, and doctors can provide telemental health services.
Telemental health services take place over the internet or phone, and patients can access these services from remote locations.
Mental health symptoms, emotional distress, struggles with relapse, and behavioral problems can be addressed through telemental health services.
In most cases, psychiatrists and psychologists, counselors, and therapists offer telemental health services.
Telemental health services are ideal for people who reside in remote locations and may not have access to a team of experienced healthcare workers in their area. Also, patients who don’t have access to reliable transportation can benefit as well.
For severe cases of addiction and mental health disorders, telemental health services is not sufficient enough care. Clinicians also can’t examine patients, and it can be easier for patients to hide their symptoms from a doctor they only communicate with through a screen.
Patients who reside in rural communities and patients who do not have immediate and convenient access to transportation can have significant difficulty accessing affordable care that can meet their dual diagnosis needs. For these patients, access to telemental health services can be a godsend. These services have dramatically increased patient’s access to care for psychiatric and psychological services.
Acute residential treatment is a highly structured environment for people with severe drug addiction disorders.
Acute residential treatment programs usually last for several weeks. The goal of the treatment is to get the patient stabilized from severe detox and withdrawal symptoms.
These treatment programs are subject to state licensing requirements.
An acute residential treatment center is located in a hospital setting.
Severe drug and alcohol detox symptoms are addressed in an acute residential treatment program.
Patients are given access to a team of skilled doctors and nurses who can help them maintain sobriety after initial detox. Patients are typically prescribed medications to blunt the effects of withdrawal and are monitored for health problems that can arise after the withdrawal timeline.
Acute residential treatment programs keep patients safe from harmful outside influences. These programs are also effective for preventing a relapse.
These treatment programs are restrictive and disruptive to a patient’s life.
Acute residential treatment is similar to the level of care provided in inpatient rehab programs and treatment facilities. This type of care offers patients a highly structured environment with 24-hour access to doctors and mental health professionals. These treatment programs are ideal for people who have safely detoxed from drugs, and who are not suffering from acute and severe mental and emotional distress, such as psychosis, or delusions. Acute residential treatment centers are for stable patients who need continuous behavioral and medical supervision before they transition to a less structured rehab program.
IOPs are designed to help people maintain sobriety from drugs or alcohol.
Standard outpatient care may work for some, but people with more significant needs may require intensive outpatient services, which are offered for at least nine hours per week for adults and six hours per week for adolescents. These services can meet the more intensive needs of people who have co-occurring conditions, such as an addiction and mental health disorder. Services may occur during the evenings or weekends, during the day, or before/after school.
IOP programs are subject to state licensing requirements.
IOP services usually take place in a clinical setting, hospital, or rehab program.
These programs address the patient’s needs regarding their ability to maintain sobriety.
IOPs offer counseling and therapy for patients. Patients will typically attend a range of one-on-one, group, and family therapy sessions. Recreational activities, career counseling, and support groups may also be offered as part of an IOP.
IOPs are less costly than inpatient treatment or PHP programs. They offer patients more flexibility in the treatment schedule as well.
Patients who are in an IOP may be tempted to use outside of the facility. They also will not have access to their counselor when they may need guidance.
An IOP is sometimes the first step in the treatment process for people with addiction and mental health disorders. These programs are typically suitable for patients who are not a danger to themselves or others, and can safely live at home while going through detox, withdrawals, and stabilizing from mental health disorder symptoms.
A person in an IOP program may need to attend a rehab facility for up to 8 hours per day, where they can receive detox medications and are also under the care and supervision of doctors and mental health professionals. Patients are required to attend therapy, and other activities are also available for patients, such as yoga, meditation, and group recreational sports. Intensive outpatient programs are ideal for people with caregiving responsibilities, and some IOP programs may even offer onsite childcare. The main difference between an IOP program and a general outpatient program is that IOPs tend to be far more structured, and patients are required to be on site for more extended periods during the day.
Drug replacement centers are for people in recovery from opioid addiction.
Opioid addiction is a severe, chronic disorder. Patients may need to use drug replacement therapy for years after achieving initial sobriety.
These facilities must comply with a variety of different state licensing and regulation requirements.
Drug replacement centers are typically located in urban areas throughout the U.S. They may be part of a hospital or other private clinical facility or rehabilitation facility.
Drug replacement centers administer replacement medications designed to help curb opioid cravings and also prevent a person from getting high if they relapse.
These centers offer medication-assisted treatment (MAT), and they typically prescribe either buprenorphine or methadone. Some centers may also prescribe naltrexone. While drug replacement centers typically treat opioid addiction, it is helpful to understand that medications are available to help treat alcohol addiction as well. These include acamprosate, disulfiram, and naltrexone.
Taking an opioid replacement drug can significantly decrease the risk of relapse for recovering addicts. Replacement drug therapy also lessens withdrawal severity and blocks an opioid high if a person retakes a drug. Drug replacement therapy can also prevent people from injecting heroin, reducing their risk of contracting HIV or hepatitis.
Unfortunately, opioid replacement drugs come with a risk of addiction. Taking an opioid replacement drug long term can also negatively impact liver function.
Drug replacement and maintenance therapy are extremely beneficial for managing opioid addiction and preventing relapse. Opioid drugs are some of the most addictive substances in the world, and maintaining initial sobriety from opioid addiction is challenging. Part of recovery from opioids means dealing with incredibly intense cravings. Numerous studies have proven that replacing an opioid drug with a legal, safe medication designed to curb cravings and lessen withdrawals is a vital part of maintaining sobriety for people in recovery from this addiction. Replacement drugs can also prevent a fatal overdose if someone relapses while in recovery for opioid addiction.
Some of the most common replacement drugs for opioid addiction are methadone and buprenorphine. Patients who are prescribed these replacement drugs must obtain them through a drug replacement center, and patients are usually limited to obtaining only a daily dose of the medication each time they visit the center since these replacement medications also come with a slight risk of addiction and abuse.
Addiction and mental health disorders can trigger and worsen each other’s symptoms. For patients and their loved ones, access to integrated, customized treatments, support, and encouragement from loved ones and medical professionals is crucial to the recovery process.
If you are looking for addiction or mental health treatment in Southern California, Mission Harbor Behavioral Health has locations Santa Barbara and more locations, and we offer multiple levels of care. Our services include partial hospitalization as well as intensive outpatient services. We also have an outpatient program for adolescents. We offer various treatment tracks, including services for substance abuse and mental health. In addition, we can provide a working professionals program to meet the needs of those who are balancing the demands of treatment and work. Mission Harbor is proud to accept multiple insurance providers to cover the cost of treatment. Contact us today to determine the best option for you.
Updated content on 4/27/2021
This guide is intended to be informational. If you are considering help for you or your loved one and would like more information, please consult a medical professional or licensed treatment facility.

