In this guide:
- What does the “evidence” refer to in an evidence-based treatment practice?
- What are some examples of evidence-based treatment methods for mental health and substance abuse?
- What are the most significant benefits of evidence-based practices that patients and clinicians experience?
- What is the difference between EBP and non-evidence based practices?
- What is the controversy surrounding either type of treatment method?
- What are some popular therapies that are not considered evidence-based?
- What are the most significant benefits of non-evidence based practices?
- Are EBPs better than non-EBPs or vice versa?
- How should EBPs and non-EBPs be used for effectively treating substance abuse and mental health issues?
- How do drug rehabilitation centers blend EBPs and non-EBPs for maximum effectiveness?
When searching for healthcare services, people will often come across the terms “evidence-based” or “empirically supported practices.” Evidence-based practices refer to an intersection of clinical, scientific evidence, patient values and preferences, and provider experiences. Evidence-based practices are used across the medical field to treat patients with a variety of adverse mental health and behavioral health conditions. But the debate between evidence and non-evidence based treatment methods is ongoing.
 In the late 1990s, Dr. David Sackett referred to evidence-based medicine as, “The conscientious, explicit and judicious use of current best evidence in making decisions about the care of the individual patient. It means integrating individual clinical expertise with the best available external clinical evidence from systematic research.”
In the late 1990s, Dr. David Sackett referred to evidence-based medicine as, “The conscientious, explicit and judicious use of current best evidence in making decisions about the care of the individual patient. It means integrating individual clinical expertise with the best available external clinical evidence from systematic research.”
Dr. Sackett also referred to evidence-based medicine as a three-legged stool. Patient values and preferences comprised one leg of the stool and scientific evidence, along with provider experiences, made up the remaining two legs of the stool of evidence-based medicine. The following guide will explore the three legs of the stool in more detail, and list common evidence-based practices (EBPs) and non-evidence based practices in the field of mental health and substance abuse rehabilitation.
In the 1990s, the term evidence-based treatment entered the field of medicine and was used as a call for using critical thinking skills when administering a treatment method. The evidence refers to clinical studies to bolster the treatment efficacy. When it comes to EBPs, clinicians are urged to use therapies that are based on the scientific method. Of course, throughout their practice, clinicians can use other ways of interacting with and effectively treating patients with new and innovative approaches that haven’t necessarily been put to a clinical trial. Even established EBPs did not start with a clinical trial, but with the practice and experimentation of innovative clinicians and the support of their patients.
The scientific method uses real-world testing methods on new ideas. Science is therefore used as a tool to help find what works for some patients based on specific metrics and settings. It is not, however, used to be closed-minded about what kinds of treatments can work for patients.
Evidence-based methods are continually being expanded upon and improved with new innovative treatment methods because science and medicine are always evolving. Doctors, therapists, and other clinicians are routinely exploring new ways to interact with and treat their clients. Evidence-based medicine, and the scientific method that bolsters it is a way to test and tweak treatment methods for maximum effectiveness continually.
What are some examples of evidence-based treatment methods for mental health and substance abuse?
The National Alliance on Mental Illness defines an evidence-based practice as one that has been researched scientifically or academically. The exercise has been proven effective and replicated by at least two or more studies. Also, the evidence-based practice must integrate both medically-based research along with individual patient values and the experiences of the clinical provider, creating Dr. Sackett’s three-legged stool.
Some common mental health and drug abuse treatment methods that are considered EBPs are as follows:
- Cognitive Behavioral Therapy
- Exposure Therapy
- Functional Family Therapy
- Assertive Community Treatment
- Dialectical Behavior Therapy
- Motivational Interviewing
- FDA-approved Medicines
Each of these methods has been proven effective through a range of clinical settings, but one of the most effective and well-known EBPs is Cognitive Behavioral Therapy or CBT. CBT is highly effective at treating a variety of mental health disorders and addiction and substance abuse, too.
As a therapy, CBT works by helping people uncover the complex relationships that surround and feed into their negative thoughts, feelings, and subsequent self-destructive behaviors. CBT is an active intervention method that seeks to re-shape positive influences in brain chemistry by changing the way patients think about themselves and their surroundings. Furthermore, there is extensive evidence available that bolsters CBT’s effectiveness.
What are the most significant benefits of evidence-based practices that patients and clinicians experience?
When it comes to using an EBP as a part of a patient’s treatment regimen, doctors and clinicians can rest assured that the treatment is most likely to work. With numerous studies and other pieces of evidence to prove the treatment’s effectiveness, patient’s can quickly find relief with EBPs. Most studies that are used to back-up EBPs involve thousands of patients in large-scale, sophisticated clinical studies. The risk factors have already been assessed, saving clinicians and patients precious time to get the patient the relief from mental health issues and drug addiction that they need.
In addition, most EBPs include thorough instructions and plans that can be easily replicated for patients. Because these methods have been proven to work time and time again, and they are standardized, care is usually less expensive than more experimental, cutting-edge treatment methods and practices.
Patients also have the added benefit of knowing that most EBP clinicians are highly-trained, experienced, and knowledgeable. They have the necessary tools on hand to help patients quickly improve their quality of life and overcome drug addiction and mental health symptoms effectively. Since clinical expertise is one of the legs of the EBP stool, therapists who utilize EBPs have particular areas of specialty. Patients may find it beneficial if a therapist has substantial experience with treating a specific disorder, for example, depression with comorbid substance abuse.
The Journal of Psychiatric Services claimed in a recent study that EBPs are more effective than traditional healthcare methods, too. EBPs use an approach that is integrated into helping patients improve different, important facets of their lives simultaneously, such as their lifestyles, habits, relationships, and their ability to become independent.
For people with substance abuse disorder who use an effective EBP such as CBT, they are encouraged to seek out family and peer support, learn their unique stressors and triggers, and implement plans and habits to avoid a drug or alcohol abuse relapse. EBPs suggest that the most effective way to treat and manage drug addiction is through lifestyle changes and behavioral modification after the initial detox phase.
With EBPs, patients are able to improve in all areas of their lives. EBPs are especially helpful for drug addicts who enter recovery. Up to half of all people who enter drug rehab suffer from a comorbid mental health condition. While it’s crucial for the patient to successfully detox, they must go on to receive an integrated treatment method to prevent a relapse. This is one area in which EBPs are most effective. EBPs can treat the addiction and the comorbid mental health condition at the same time.
What is the difference between EBP and non-evidence based practices?
Traditional, non-evidence based practices rely on the rapport between the clinician and the patient, and less on the scientific evidence of the practice if there is any. This type of exercise is highly individualistic. Traditional treatment methods tend to heavily rely on the patient’s individual preferences and the therapist’s personal experiences with the treatment method. In some cases, clinicians may find their own experiences in the medical field to be more reliable than EBPs. When it comes to non-evidence based treatment methods, medication and the patient’s thought processes and preferences are the most critical factors to the treatment process.
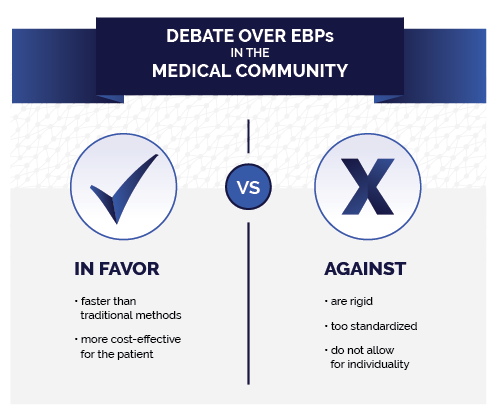
There is an ongoing debate in the medical community between evidence-based practice clinicians and proponents of traditional treatment methods. Those in favor of conventional methods argue the following:
- That EBPs are rigid, too standardized, and do not allow for individuality.
- Clinical studies may not be broad enough, and minorities may lack adequate representation.
Those arguing in favor of EBPs claim the following:
- EBPs tend to work faster than traditional methods
- Faster treatment is, therefore, more cost-effective for the patient
The most popular non-evidence based practices for mental health and substance abuse disorder are:
- 12-Step Programs
- Conversion Therapy
- Talk Therapy
Traditional, or talk therapy is a highly individualistic treatment method that uses the relationship between the therapist and the patient to uncover subconscious and conscious issues related to substance abuse.
In many cases, clinicians will also prescribe FDA-approved medications in conjunction with talk therapy. This is a common and effective way to use both EBPs and non-EBPs to help people with substance abuse and comorbid mental health issues. In addition, 12-step programs are effective ways to build supportive relationships with people who also struggle with substance abuse issues.
What are the most significant benefits of non-evidence based practices?
With traditional treatment methods, care is highly individualized. Patients have the added benefit of building a rapport with the clinician, where it is easier to tweak and modify the treatment method for the patient’s specific needs. With 12-step programs, patients are able to forge supportive relationships with people who are experiencing similar struggles. Human relationships are at the core of traditional treatment methods, and as such, they aren’t something that can be reduced to a scientific formula that can be replicated across the board.
Are EBPs better than non-EBPs or vice versa?
One is not necessarily better than the other. Despite the ongoing debate between the two fields study within the scientific and medical communities, there is no clear-cut evidence that one is better than the other. However, science and medicine are continually evolving. The most effective way to treat patients with substance abuse disorder and comorbid mental health conditions is with a combination of both types of treatment methods.
How should EBPs and non-EBPs be used for effectively treating substance abuse and mental health issues?
Both types of treatment methods should be blended and matched to the individual patient. Drug abuse and mental health issues are highly complex problems that tend to feed into each other and worsen the effects of each. By taking well-known, scientifically-backed methods and blending them with traditional individualized methods, patients can obtain highly-effective, customized care for both substance abuse and mental health problems.
There are several steps that those who enter rehab must take to treat and manage drug addiction along with a comorbid mental health condition. The initial phase of treatment usually involves a medically-supervised detox. Here, patients participate in EBPs to safely withdrawal from the substance. They may require FDA-approved maintenance medications, or other prescription and OTC drugs to counteract the dangerous effects of withdrawal.

After a patient has safely detoxed from drugs or alcohol, they must begin the work of managing their substance use disorder along with any comorbid mental health conditions for ongoing, lifelong sobriety. At this phase of the treatment, most rehabilitation facilities will blend together EBPs and non-EBPs.
Patients may require CBT or DBT depending on their conditions. Talk therapy, family therapy, group therapy, and 12-step programs also help patients learn more about their triggers and the negative emotions they feel that contribute to their drug-use tendencies. In these different types of therapies, patients build a supportive relationship with therapists and also learn safe, effective, and proven ways to manage their triggers and emotions.
For patients with a comorbid mental health condition, they will also need prescription medications in tandem with therapy. Medications are FDA-approved and are considered an EBP. Ongoing or aftercare treatment plans are also put into place. These plans are highly individualized, blending both evidence-based and non-evidence based practices. Patients will often continue with prescription medications, support groups, and therapy to manage their condition and prevent a relapse.
Substance abuse disorders and mental health conditions do not have a cure, but they are not life sentences, either. With effective, tailored treatment plans that blend the best of both the EBP and the non-EBP world, patients are able to manage adverse mental health and behavioral conditions and achieve lifelong sobriety from drugs and alcohol. For people who struggle with these conditions, there are hundreds of safe, supportive, and proven-effective rehabilitation centers across the country that can help them recover from substance abuse and mental health issues. By blending both treatment methods, patients have the highest chances of success.
This guide is intended to be informational. If you are considering help for you or your loved one and would like more information, please consult a medical professional or licensed treatment facility.

