In this guide:
- At what rate do first responders abuse drugs and alcohol?
- How do trauma and stress-related mental health disorders affect first responders?
- How is PTSD diagnosed?
- What is the most commonly abused substance amongst first responders?
- Is there help available for first responders suffering from PTSD and substance abuse disorders?
- How does the treatment process begin?
- The specific goals of treatment for first responders
- A List of Resources for First Responders
Police officers, firefighters, and paramedics deal with high levels of trauma and stress in their day-to-day working lives. But what happens when the person who helps others first is in need of care themselves? First responders have to handle dangerous events nearly every day, and in some cases, the stress of their jobs can quickly take a toll on their mental health. Adverse mental health conditions also lead vulnerable first responders to turn to drugs and alcohol to cope with and mask their pain. The culture surrounding the job of a first responder makes these individuals more resistant to treatment than the general population, compounding the problem.
People employed in these professions often use alcohol to deal with stress. Police, firefighters, and EMTs will use alcohol as a way to promote social interaction and unwind from a stressful, or traumatic situation they’ve witnessed. The combination of socialization and alcohol further increase the risk of first responders developing a substance use disorder. The following guide will address the statistics surrounding first responder drug and alcohol abuse rates, and where first responders can turn to for help.
Emergency medical responders are at particularly high-risk of abusing alcohol. EMTs also report higher levels of post-traumatic stress disorder than the general population. PTSD can develop even if the first responder was not personally threatened. Witnessing severe, traumatic events can increase the risk of contracting PTSD. Untreated PTSD is a significant contributing factor to drug and alcohol abuse rates and other mental health conditions such as depression.

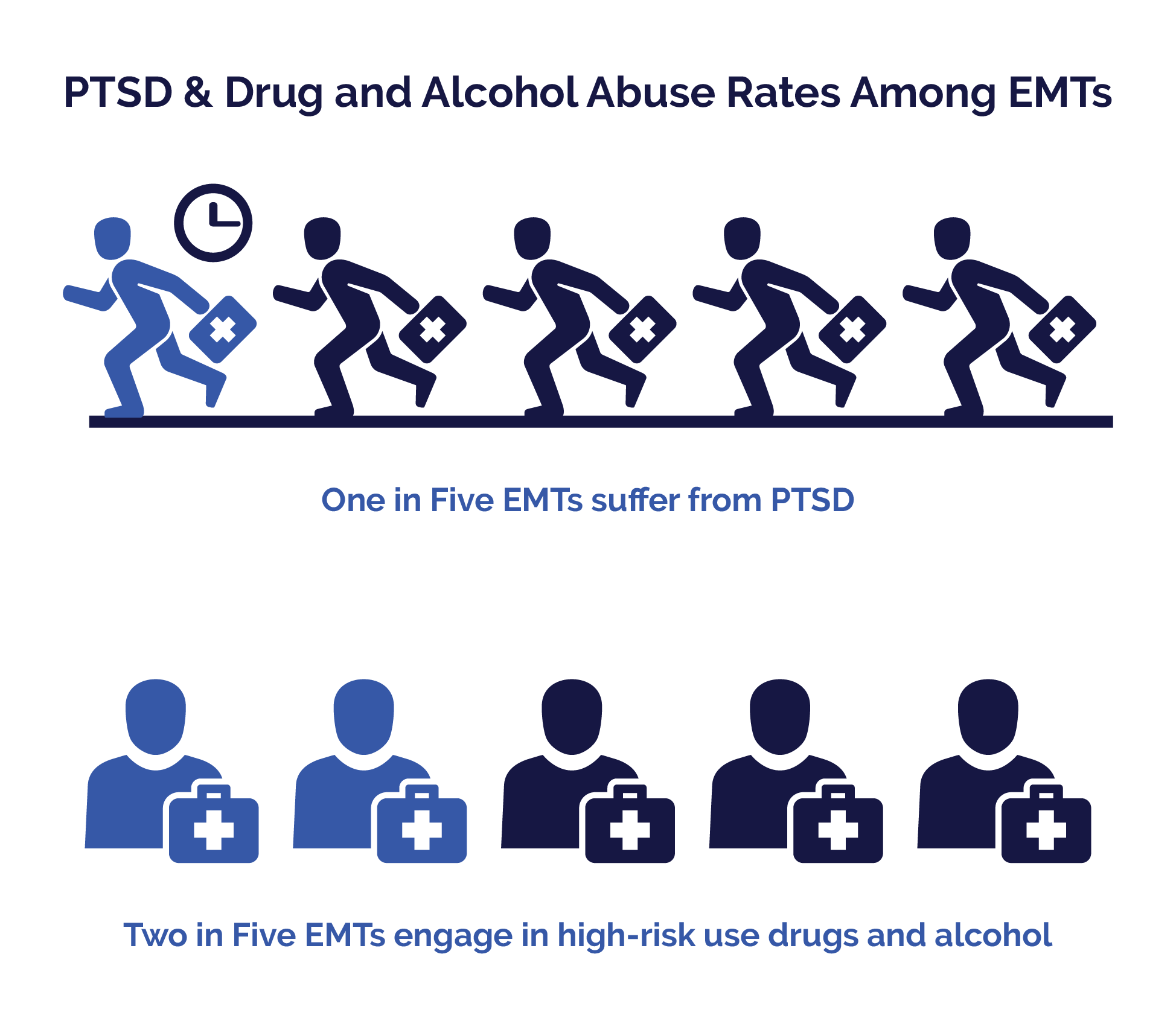
- 20% of EMTs suffer from PTSD
- 40% of EMTs engage in the high-risk use of drugs and alcohol
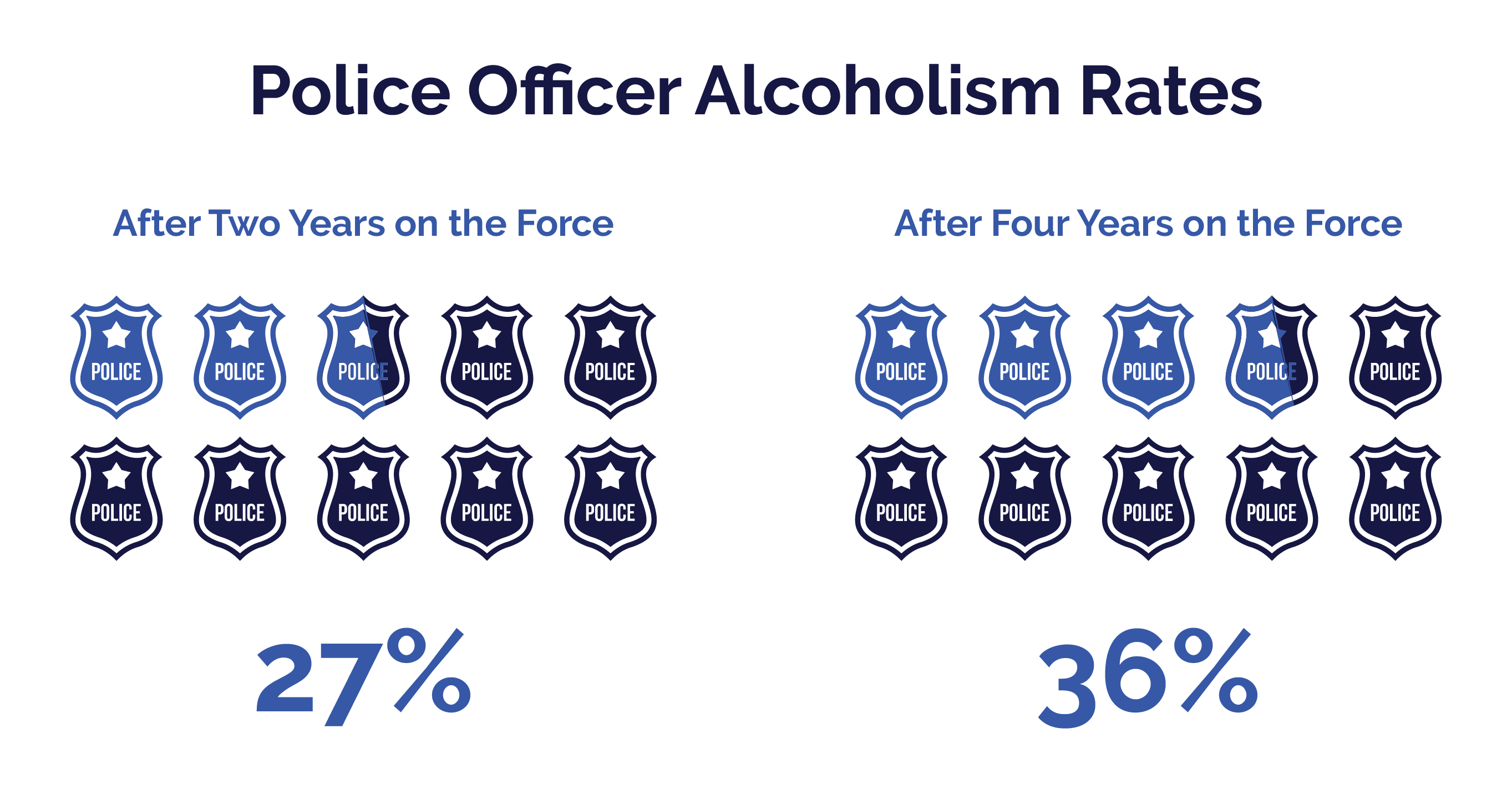
Police officers’ risk of developing an alcohol dependence increases the more years they are on the force. A recent study from the University of Arizona found that alcohol abuse and addiction rates increased the longer the study participants worked as police officers. Rookies who join the force and report 0% will experience an accumulation of job stress. After two years, 27% of rookies go on to develop an alcohol use disorder. After four years on the force, that number increases to 36%. The study also found that alcohol use is a deeply ingrained part of police force culture.
- 25% of police officers report drinking to feel like ‘part of a team.’
- 25% of police officers were negatively affected by a co-worker’s drinking
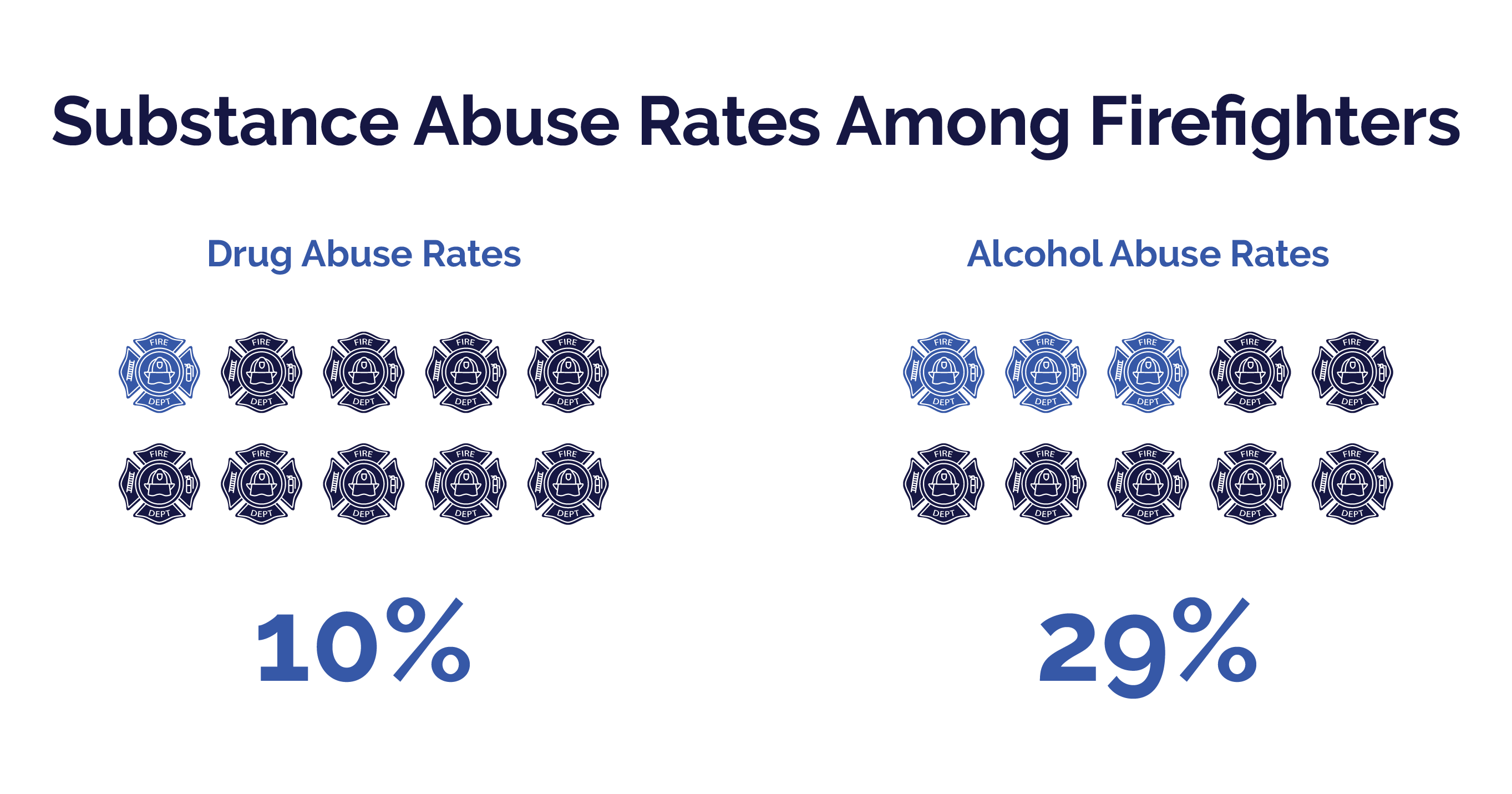
The U.S. Firefighters Association estimates that 10% of all firefighters abuse drugs. 29% of firefighters abuse alcohol. Compared to statistics in 2013 which indicated that 6.6% of the general population abused alcohol.
How do trauma and stress-related mental health disorders affect first responders?
When it comes to stress-related mental health disorders, first responders are at exceptionally high risk of suffering from them. There are several different kinds of stress and trauma-related disorders, but first responders tend to develop either PTSD or acute stress disorder.
PTSD is a chronic response to trauma or stress. Acute stress disorder is diagnosed if an individual displays similar symptoms to PTSD for one month or less after a stressful or traumatic event. Usually, the symptoms of acute stress disorder will resolve on their own within a month. PTSD-like symptoms are a rational response to an abnormal event. In some cases, people who are suffering from acute stress disorder will use alcohol in excess or even binge drink. But they usually won’t go on to develop alcohol dependence.
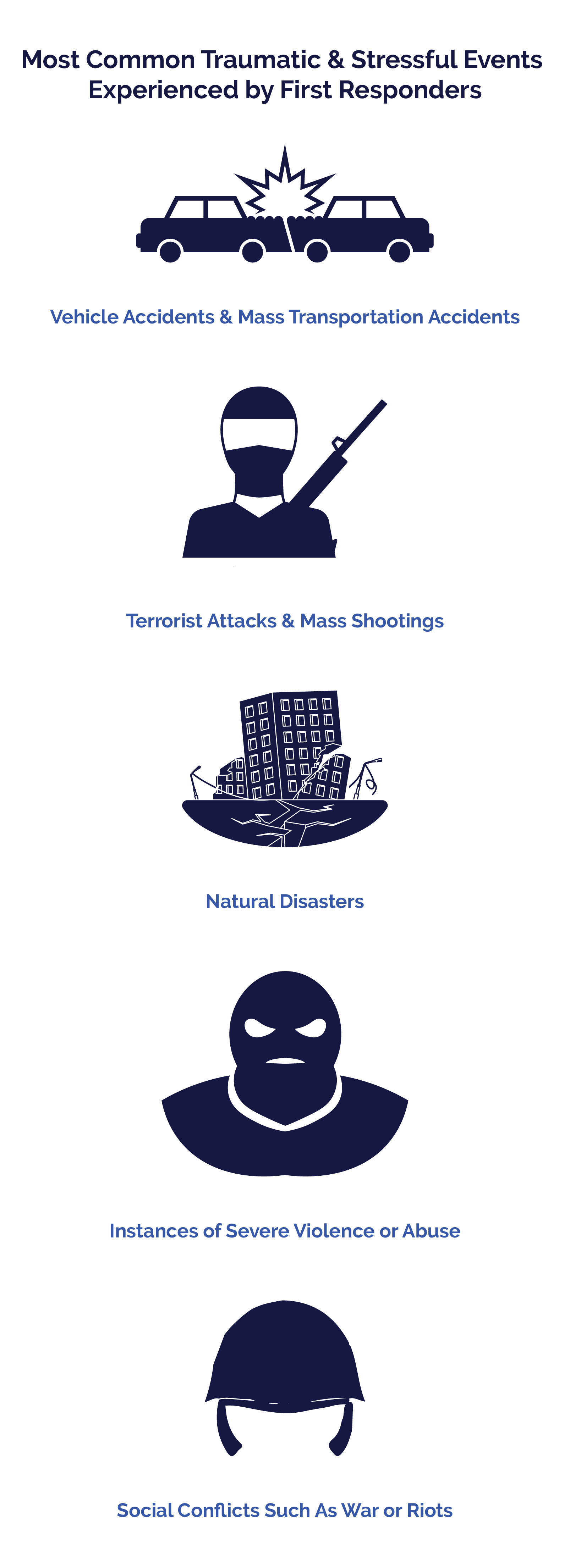
Unfortunately for some first responders, the symptoms of acute stress disorder will not fade and dissipate with time. PTSD will start to develop. A specific set of distressing symptoms characterizes PTSD. If the signs of acute stress do not go away within four weeks and begin to get worse, then PTSD is most likely to blame. Remember, a person does not have to be directly exposed to a traumatic event in order to develop PTSD. A person can get PTSD if they witnessed the incident, or have seen the aftermath of the event. The most common traumatic and stressful events that first responders can experience include:
- Vehicle accidents and other accidents involving mass transportation, such as airlines or trains.
- Terrorist attacks and mass shootings
- Natural disasters
- Witnessing instances of severe violence or sexual abuse
- Seeing social conflicts such as riots or acts of war
Only a trained medical professional can diagnose PTSD. PTSD comes with a cluster of symptoms to effect a diagnosis. Signs must be present for four weeks or more and severely affect a person’s quality of life. Untreated PTSD can lead to increased instances of alcohol or drug abuse to numb the distressing symptoms. PTSD can also precipitate a depressive episode. Symptoms include the following:

- Reliving a past traumatic event, either through vivid memories, recurring dreams, or flashbacks
- Experiencing symptoms of anxiety when the person is confronted with people, places, or things that otherwise remind them of the traumatic event
- The person goes out of their way to avoid any reminders of the traumatic event.
- Being hypervigilant of similar types of events
- Developing symptoms of depression, such as anxiety, loss of motivation, or social isolation
- Problems with focus and memory
- Feelings of detachment from others or reality
- Participating in self-destructive behavior such as substance abuse or binge drinking
- Failure to perform self-care or committing self-harming behaviors
- Pessimism and hopelessness
There is a common misconception in society that PTSD will develop soon after the traumatic event. This isn’t true. Sometimes, PTSD symptoms won’t develop for several weeks, months, or sometimes years after the fact. This is especially true with first responders. The reason why is because traumatic events can have a cumulative effect on the witness or participants. First responders are in a position where they will experience numerous and varied types of stressful, traumatic events over a period of years. In some cases, it isn’t until the first responder witnesses their tenth domestic violence case that they go onto develop the symptoms of PTSD. They may experience flashbacks of earlier traumatic events from years prior.
Of all first responders, studies estimate that between 15% and 30% have PTSD.
And recent research suggests that 20% of all first responders with PTSD have a substance use disorder. First responders who experience flashbacks and nightmares related to the traumatic event are at higher risk of abusing drugs and alcohol compared to people with PTSD who do not deal with many re-experiencing symptoms.
Alcohol is the most commonly abused substance of first responders with PTSD. There are many different reasons for this, and chief among them is that alcohol and drinking are socializing events. First responders who share the witnessing of traumatic events will often drink together as a form of stress relief and a way to bond over the trauma. Also, alcohol is a central-nervous-system depressant. Its use can dull the anxiety people feel surrounding their traumatic event. Alcohol is also easy to obtain and access across all socioeconomic levels. PTSD and alcohol abuse are also bidirectional. Developing PTSD can lead to a substance abuse problem, and those who abuse substances are at high risk of later contracting PTSD. First responders are less likely than the general population to abuse illicit drugs. Other substances that are commonly abused amongst first responders are:

- Marijuana and related cannabis products
- Opiate painkillers
- Benzodiazepines
Fortunately, there are hundreds of rehabilitation centers across the country that are tailored for individuals who have substance abuse issues with co-occurring mental health problems. When someone presents with drug or alcohol dependence in addition to a mental health condition, both disorders must be treated at the same time for the treatment to be effective. Failing to treat PTSD will only exacerbate the substance use disorder and vice versa. When both diseases are adequately addressed and treated at the same time, this is called an integrated treatment program. Integrated treatment programs combine mental health professionals and drug counselors from different backgrounds to treat the patient according to their expertise successfully. These specialists form a team of experts who are vested in offering the patient-tailored treatment plans that address all aspects of their substance abuse disorder and mental health condition. Usually, the team is comprised of therapists, counselors, social workers, psychiatrists and physicians who are all well-versed in treating co-occurring disorders.
First, trained professionals such as physicians and psychologists, and intake workers will evaluate and assess the patient at all levels. At this stage, a proper diagnosis is given, and the team will assemble to develop a customized treatment plan for the patient. Throughout treatment, the team is in communication, and they will document the patient’s progress and make any adjustments to the program as needed.
Integrated treatment plans are part of a long-term commitment that the patient makes to manage their condition. With integrated treatment, the patient’s social, psychological, and physical needs are addressed and met. Patients are often treated with a precise combination of therapy, social support, and pharmacological interventions.
First responders who enter a treatment program with co-occurring PTSD and drug abuse will often need to undergo a medical detox regimen, followed by inpatient care at a rehabilitation center. In most cases, inpatient care includes cognitive behavioral therapy sessions that are designed to assist the person through the withdrawal process, lessen their symptoms of anxiety and depression, and reduce their cravings for drugs or alcohol. Medications alone cannot help someone through recovery, and they will need a combination of CBT and group therapy sessions to recover. Research indicates that first responders in particular benefit from social support groups where the members are also part of the first response professions.
- Help the person express their needs in a way that doesn’t lead them to feel inadequate, vulnerable, or exposed.
- Enable the patient to develop stronger ties with a social support system.
- Help the patient strengthen family bonds through family therapy sessions.
- Assist the first responder with developing healthy interests outside of work that helps them de-stress from the intense nature of their job.
- Encourage the patient to continue participating in therapy and educational classes that help them recognize the signs of traumatic stress and cravings for alcohol or drugs.
Barriers to Seeking Help Among First Responders
While there are services available to help first responders struggling with addiction, the reality is that some firefighters and police officers may be hesitant to seek help. According to a recent study, some barriers that may stand in the way of getting treatment for an addiction included the following:
On the other hand, first responders who had positive experiences with a therapist, knowledge of treatment, and a realization that they were not alone were more likely to engage in treatment. This means that first responders need access to training on the rates of substance abuse in their profession and information about available drug and alcohol treatment resources in their community. Given that first responders may feel obligated to care for their families instead of caring for themselves through treatment, they must be referred to services, such as outpatient treatment, that allow them to continue to work and be present with their families, if possible.

If you are a first responder yourself, remember that you are working in a stressful job, and sometimes, using drugs or alcohol becomes a coping mechanism for trauma. This is a relatively prevalent problem among first responders, and asking for help is not a sign of weakness. Instead, it shows that you are willing to get the treatment you need to recover and be the best you can for your coworkers and your family. Remember, you cannot care for your family or the community if you do not first care for yourself. Also, keep in mind that healthcare providers, including addiction treatment professionals, are legally required to keep your personal information confidential.
- There are 16 fire stations in Santa Barbara County, California with educational resources available on their websites.
- The Employee Assistance Programs offer referrals and classes for people with high levels of stress and substance abuse issues.
- The Substance Abuse and Mental Health Services Administration offers a list of treatment provider locations.
- The PTSD Foundation of America also has several resources available for first responders on their website.
- Alcoholics Anonymous also offers local meetings that cater to specific demographics.
- The National Suicide Prevention Hotline is a toll-free number where individuals thinking of self-harm can call for help any time, day or night.
- The Salvation Army also offers a list of treatment centers that individuals can call for help with substance abuse and mental health issues.
First responders with substance abuse disorders and trauma-related mental health problems need to remain in treatment long enough to develop an adequate coping mechanism for stress and work-related trauma. To prevent a recurrence of PTSD symptoms and substance abuse, first responders will need assistance from trained professionals on how to recognize and prevent triggers. Treatment is designed to provide first responder patients with the tools necessary to deal with PTSD and substance abuse disorder that is specific to their work and lifestyle. It’s crucial that first responders have ongoing maintenance plans and support groups in place to allow for a smooth transition back into treatment if they experience a relapse of PTSD or drug abuse. If you or a first responder loved one has PTSD or substance abuse, don’t hesitate to reach out for help. With a tailored treatment plan, people living with PTSD and a substance abuse disorder can go on to make a full recovery and continue saving lives and helping the most vulnerable members of society.
Addiction Services That Meet The Needs of First Responders
Since PTSD is prevalent among first responders, they are likely to benefit from trauma-informed services when they enter addiction treatment. This type of care considers the impact that trauma has on a person’s life and their progress in treatment.
For first responders seeking addiction rehab, it is crucial to choose a program that addresses trauma and uses practical approaches for treating it. According to research, programs that use a cognitive-behavioral approach to treatment effectively address co-occurring trauma and addiction. A type of counseling called exposure therapy, which involves describing a traumatic experience and processing it, can also be helpful for first responders coping with trauma and addiction.
If you or a loved one is seeking treatment for co-occurring PTSD and substance abuse in Southern California, Mission Harbor Behavioral Health is here to help. We are happy to meet the needs of first responders, and we offer an evening program for adults so you can continue to work while going through treatment. We also provide a variety of types of therapy, including trauma therapy, exposure therapy, and cognitive-behavioral therapy, so you can be sure you are getting treatment that is effective for both PTSD and addiction. Contact us today to learn more about the treatment services we offer in the Santa Barbara and Southern California areas.
Updated content on 4/20/21
This guide is intended to be informational. If you are considering help for you or your loved one and would like more information, please consult a medical professional or licensed treatment facility.

