Witnessing acts of warfare can be severely unsettling. It can also have significant mental health consequences for military personnel. Witnessing death, destruction, and torture; experiencing unexpected and at times continuous threats to one’s life; or participating in hostilities and killing can potentially lead to mental health problems.
Making this even worse, according to the Guardian, is that one in five soldiers had a common mental illness before enlisting in the army and were able to clear the military’s screening process. The disorder most associated with the study was Intermittent Explosive Disorder which points to depression.
Wars have had an important part in psychiatric history in a number of ways. It was the psychological impact of the world wars in the form of shell shock that supported the effectiveness of psychological interventions during the first half of the 20th century. It was the recognition of a proportion of the population not suitable for army recruitment during the Second World War that spurred the setting up of the National Institute of Mental Health in the USA. And over 2 million Americans have been deployed to Iraq and Afghanistan over the past decade and increasing numbers are returning home with complex mental and behavioral health challenges.
According to a report from the US National Library of Medicine National Institute of Health, studies have shown that conflict situations cause more mortality and disability than any major disease. War destroys communities and families and often disrupts the development of the social and economic fabric of nations. The effects of war include long-term physical and psychological harm to children and adults, as well as reduction in material and human capital. Death as a result of wars is simply the “tip of the iceberg”. Other consequences, besides death, are not well documented. They include endemic poverty, malnutrition, disability, economic/ social decline and psychosocial illness, to mention only a few. Only through a greater understanding of conflicts and the myriad of mental health problems that arise from them, coherent and effective strategies for dealing with such problems can be developed.
* According to a 2014 report by the Department of Defense, there were 1,080 suicide attempts (245 suicides) among active-duty service members for all armed services in calendar year 2013.
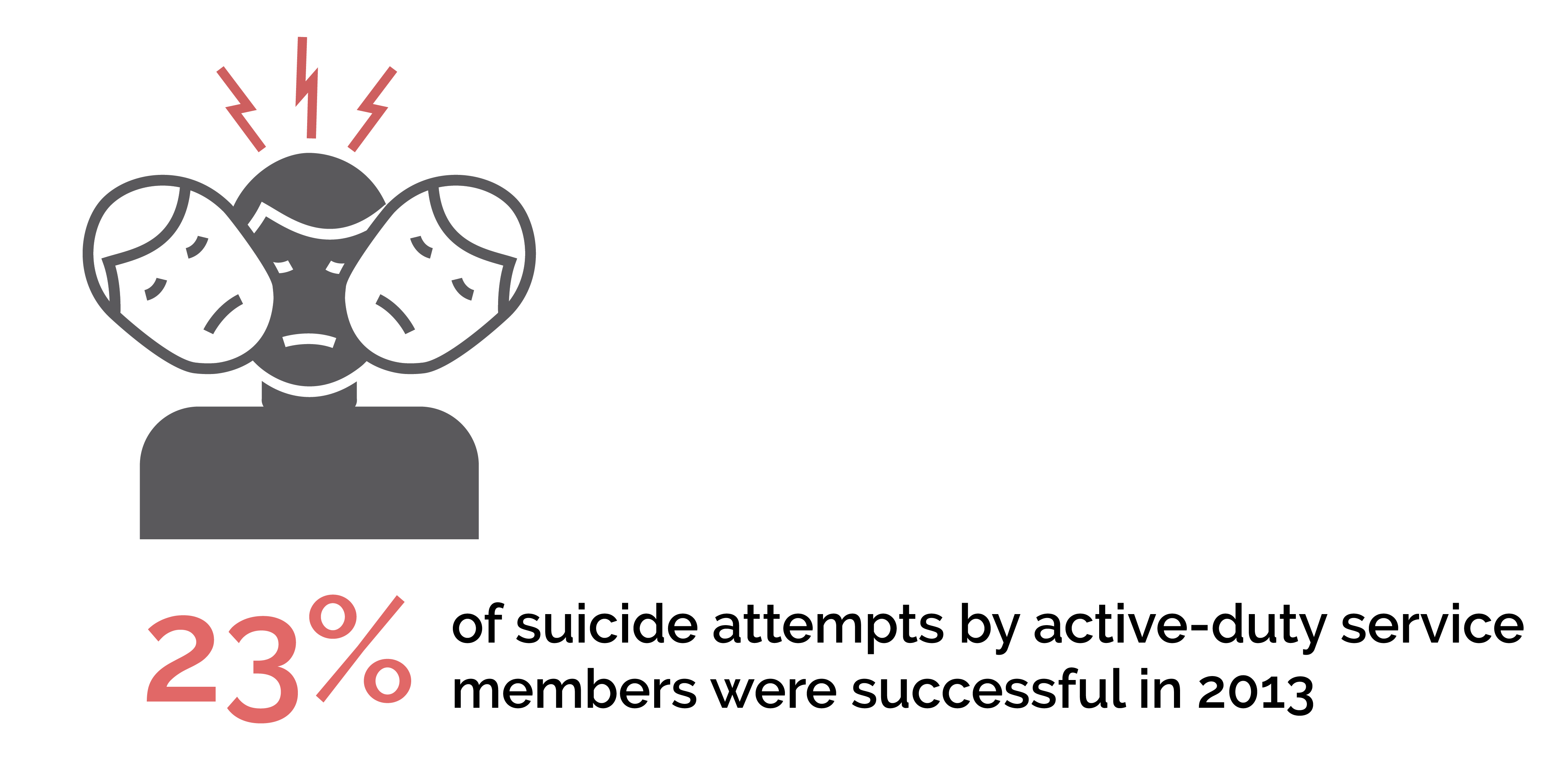
* A recent study of 52,780 active-duty members of the U.S. Air Force found that 3 percent of male participants and 5.2 percent of female participants reported suicidal ideation in the previous year. Of the participants that reported suicidal ideation, 8.7 percent also reported a recent suicide attempt.
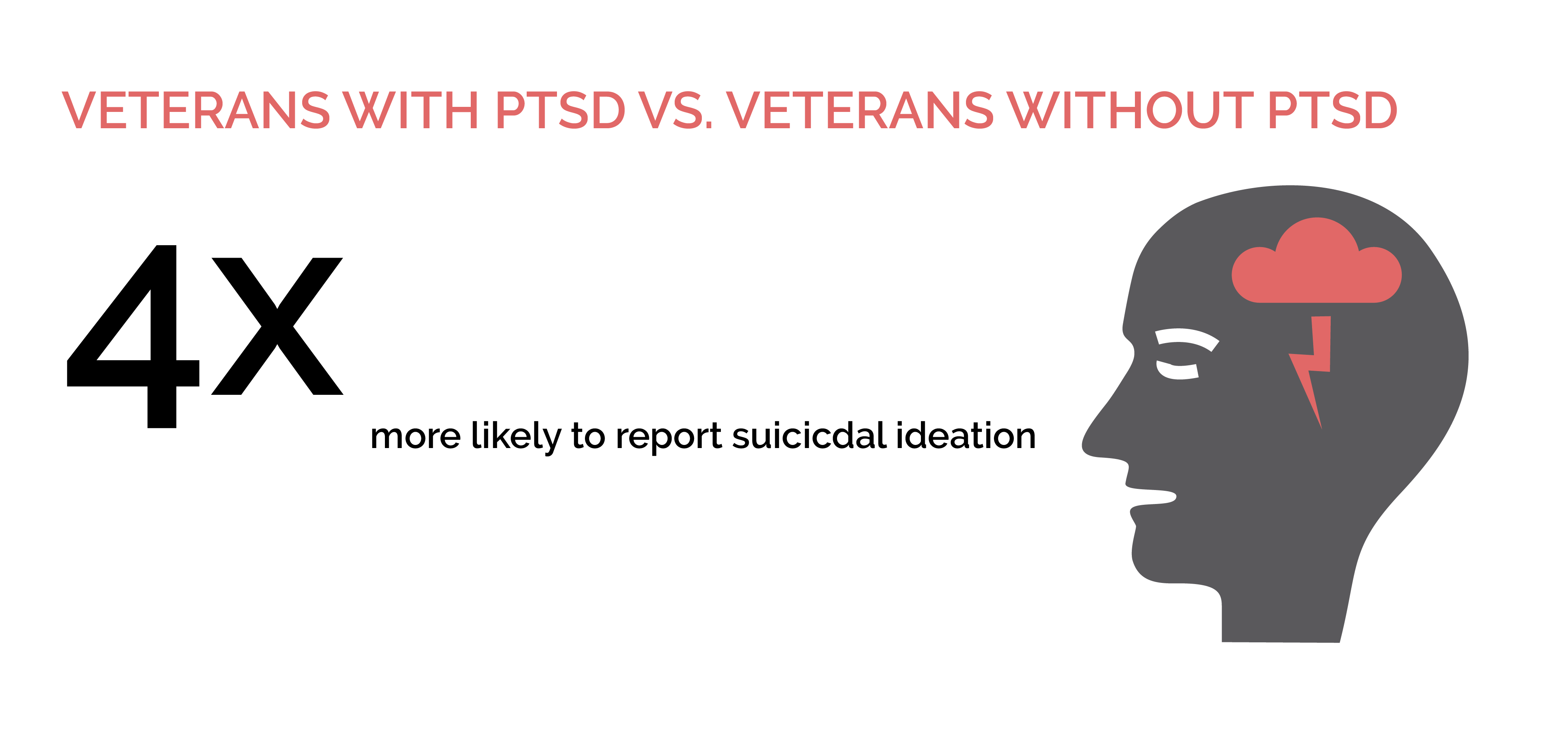
* Veterans who screened positive for PTSD were 4 times more likely to report suicidal ideation than veterans who did not, and the likelihood of suicidal ideation was 5.7 times greater in veterans who screened positive for PTSD and two or more comorbid disorders.
* Military Sexual Trauma has become an important risk factor for PTSD. National data indicate that about 1 in 4 women and 1 in 100 men responded “yes” that they experienced MST, when screened by their VA provider.
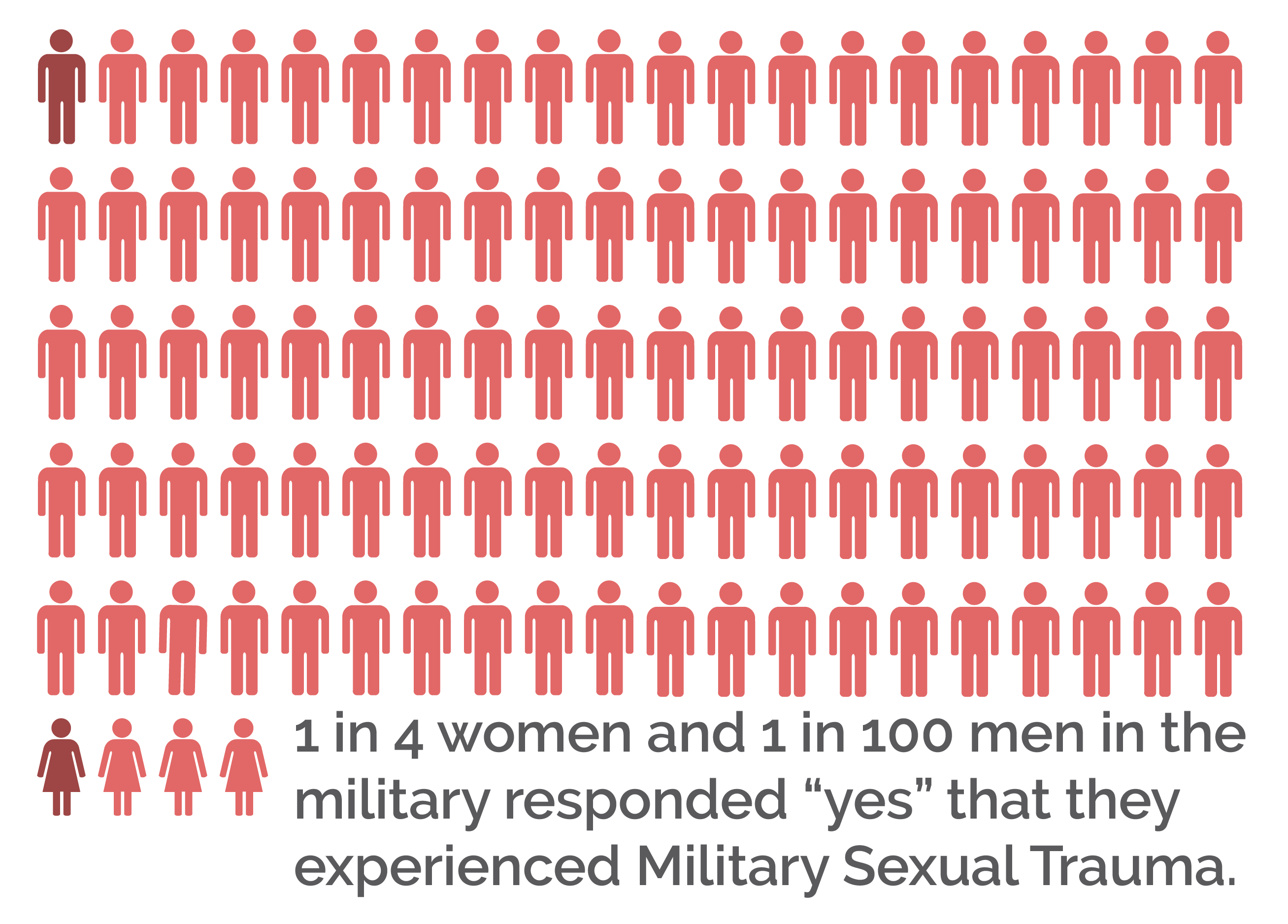
* For women, it is estimated that female veterans who have a history of MST are nine times more likely to develop PTSD compared to female veterans who had no history of sexual trauma.
* Data indicates that one-third of returning Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF) service members have reported symptoms of mental health or cognitive problems.
According to the Substance Abuse And Mental Health Services Administration (SAMHSA) there are an estimated 23.4 million veterans in the United States, and about 2.2 million military service members and 3.1 million immediate family members.
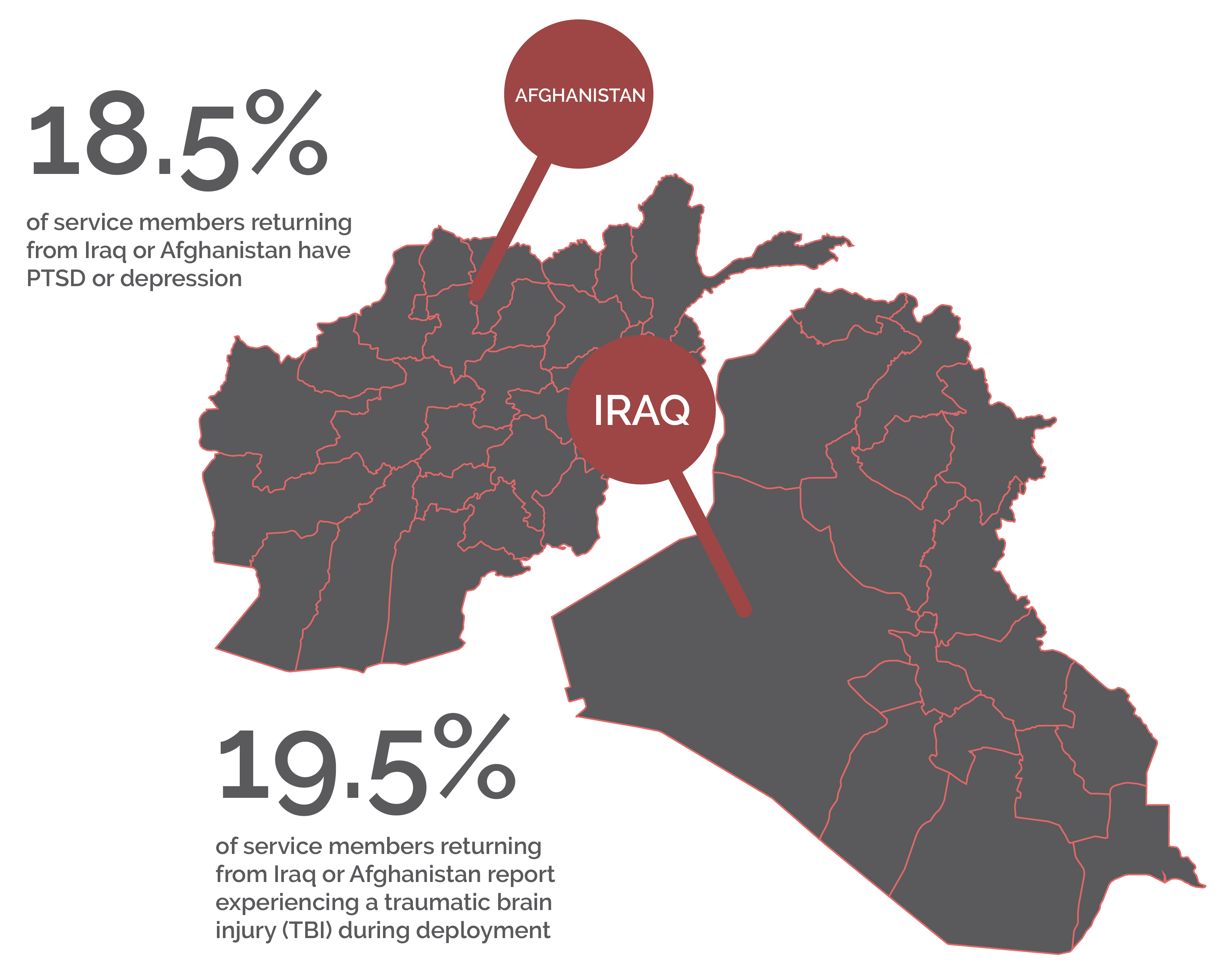
- Approximately 18.5% of service members returning from Iraq or Afghanistan have post-traumatic stress disorder (PTSD) or depression, and 19.5% report experiencing a traumatic brain injury (TBI) during deployment.
- Approximately 50% of returning service members who need treatment for mental health conditions seek it, but only slightly more than half who receive treatment receive adequate care.
- Between 2004 and 2006, 7.1% of U.S. veterans met the criteria for a substance use disorder.
- The Army suicide rate reached an all-time high in 2012.
- In the 5 years from 2005 to 2009, more than 1,100 members of the Armed Forces took their own lives, an average of 1 suicide every 36 hours.
- According to an assessment by the Department of Housing and Urban Development (HUD) and Veterans Affairs (VA), nearly 76,000 veterans experienced homeless on a given night in 2009. Some 136,000 veterans spent at least one night in a shelter during that year.
- Mental and substance use disorders caused more hospitalizations among U.S. troops in 2009 than any other cause.
- A recent Treatment Episode Data Set (TEDS) report states that about 70% of homeless veterans also experience a substance use disorder.

Here in Southern California, there is a veritable mecca of military bases. Some of them – including Vandenberg, Naval Battalion Center and NAS Point Mugu – are close to Mission Harbor. And at each are members of the armed forces in pain – people who have struggled through the horrors of war and conflict and who have internalized everything they have seen. Horrors the civilian population could not begin to understand, only having seen them vastly removed from their place of origin on television.
Greatest Risks
Nearly 1 in 4 active duty members showed signs of a mental health condition, according to a 2014 study in JAMA Psychiatry. Military service members are most at risk for:
Post Traumatic Stress Disorder (PTSD)
Traumatic events, including but not limited to military combat, assault, disasters or sexual assault have the potential for long-lasting negative effects such as trouble sleeping, anger, nightmares, and alcohol and/or drug abuse. When these troubles remain, it could be PTSD. The 2014 JAMA Psychiatry study found the rate of PTSD to be 15 times higher than civilians.
Traumatic Brain Injury (TBI)
A traumatic brain injury is oftentimes the body’s reaction to a significant blow to the head or body. Symptoms can include headaches, fatigue or drowsiness, issues with memory and changes in mood.
Depression
This is far more than just “being sad.” Depression is not a sign of weakness nor is it something a person can shrug off. It can take over your life and hurts your ability to function properly – thus, more often than not, it requires treatment. The 2014 JAMA Psychiatry study found the rate of depression to be five times higher than in civilians.
Types Of Treatment
According to Military.com, the main treatments for people with PTSD are counseling (known as “talk” therapy or psychotherapy), medications, or both. Although there are a number of treatment options for PTSD, and patient response to treatment varies.
CBT
One form of counseling is known as cognitive-behavioral therapy (CBT). This is where a therapist helps a service member dealing with PTSD understand and change how thoughts and beliefs about the trauma, and about the world, cause stress and maintain current symptoms.
Group Therapy
A group therapy session allows service members to discuss their trauma and/or gain skills that help manage the symptoms of PTSD (depending on the group). Sharing stories and connecting with others who have been through similar events can be comforting and be a great help.
Family & Couples Therapy
A therapist will help all people involved to communicate better, maintain good relationships, and cope with tougher emotions. Because of the adverse effects of PTSD on relationships, family and couples therapy can be very helpful.
Pharmacological
Selective serotonin reuptake inhibitors (SSRIs) are a type of antidepressant medication. SSRIs include citalopram (Celexa), fluoxetine (Prozac), paroxetine (Paxil), fluvoxamine (Luvox), and sertraline (Zoloft). Many, if not most, patients with PTSD will achieve some sort of symptom relief with an SSRI, although they are not as effective with combat PTSD.
Alternative Medicines
These include acupuncture, yoga, and herbal or dietary supplements, all of which have proven to have some efficacy in certain cases of PTSD.
Approximately 1.9 million OEF/OIF/OND veterans have become eligible for Veterans Affairs (VA) health care since 2002. Of these, an estimated 1.16 million veterans have registered for VA health care. Despite this, one of the problems encountered by military members includes personal barriers to care. One study found that 38% of the veterans in their sample reported a lack of trust in mental health professionals as a barrier; while 25% indicated a belief that mental health care does not work. Clearly military members need to overcome the false stigma that getting help is a bad thing.
Seventy-six percent of California veterans in need of mental health care from 2011 to 2013 either didn’t receive treatment or received inadequate care, according to a new study by the UCLA Center for Health Policy Research.
Why You Need Treatment
The Department of Defense states that leaving mental health issues untreated end up posing an even bigger safety threat than any mental health condition you need treatment for. As of 2014, discussing issues with a doctor will not and can not affect your career; even if your doctor needs to disclose the condition, there is no risk to your career.
However, by ignoring these issues and not seeking treatment is quite likely to lead to damaging or ending your career in the military. According to a 2006 study in Military Medicine, 97% of personnel who underwent treatment for mental health did not experience any negative aspects to their career. If, however, you are ordered to take a mental health evaluation, then your career will take a hit. In fact, among those who had to have a commanding officer-ordered evaluation, thirty nine percent saw a negative career impact.
The Department of Defense must follow all privacy guidelines established by both HIPAA and the Privacy Act. That way, your privacy is ensured in most situations. It won’t, however, if a doctor/health care provider realizes your condition might endanger either yourself, others, or the mission (or all three) in which case they are obligated to disclose the situation to the chain of command.
Insurance
TRICARE, once known as the Civilian Health and Medical Program of the Uniformed Services, is a health care program that provides civilian health benefits for US Armed Forces military personnel, military retirees, and their dependents. It is part of the Military Health System. In January 2018, west regions joined together under Health Net Federal Services, LLC which covers California. Health Net’s behavioral health services subsidiary, MHN, provides behavioral health, substance abuse and employee assistance programs (EAPs) to approximately 7.3 million individuals in various states, including the company’s own health plan members. The company’s subsidiaries also offer managed health care products related to prescription drugs, and offer managed health care product coordination for multi-region employers and administrative services for medical groups and self-funded benefits programs.
Any form of mental illness will hamper your ability to do your job as well as potentially harming personal relationships if not dealt with. Please seek out help before it is too late and know that there are people out there ready and willing to help you for helping us with your service.
This guide is intended to be informational. If you are considering help for you or your loved one and would like more information, please consult a medical professional or licensed treatment facility.

